| |
10:00
 |
0577.
 |
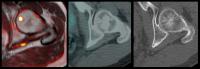
High-resolution distortion-free diffusion imaging of the
prostate using stimulated echo based turbo spin echo (DPsti-TSE)
sequence 
Qinwei Zhang1, Bram F. Coolen1, Gustav
J. Strijkers2, Laurens van Buuren3,
Uulke van der Heide3, Oliver J. Gurney-Champion 1,
Sónia I. Gonçalves4, and Aart J. Nederveen1
1Department of Radiology, Academic Medical
Center, University of Amsterdam, Amsterdam, Netherlands, 2Biomedical
Engineering and Physics, Academic Medical Center, University
of Amsterdam, Amsterdam, Netherlands, 3Department
of Radiation Oncology, The Netherlands Cancer Institute,
Amsterdam, Netherlands, 4Institute
for Biomedical Imaging and Life Sciences, University of
Coimbra, Coimbra, Portugal
Diffusion imaging is part of the standard MR imaging
protocol for prostate cancer diagnosis. Conventional echo
planar imaging (EPI) diffusion sequence has limitation on
image resolution and additionally suffers from image
distortion. The present study introduces a new stimulated
echo based 3D diffusion preparation turbo spin echo sequence
(DPsti-TSE) to achieve high-resolution and distortion free
image. The sequence is also proved to be immune to eddy
currents.
|
| |
10:12
|
0578.
 |
Detection of Aggressive Prostate Cancer Using Extradomain-B
Fibronectin Targeted MRI Contrast Agent 
Zheng Han1, Yajuan Li1, and Zheng-Rong
Lu1
1Department of Biomedical Engineering, Case
Western Reserve University, Cleveland, OH, United States
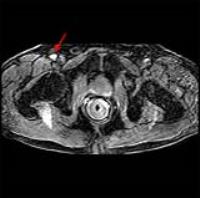
Prostate cancer (PCa) is the second most lethal cancer in
American men with a high incidence rate. Current method of
PCa screening is not specific to aggressive cancer type,
which results in overtreatment with serious adverse effects.
We developed a MRI contrast agent, ZD2-Gd(HP-DO3A), that
targets to overexpressed extradomain-B in aggressive PCa.
Our result showed an increased sensitivity for MRI detection
of aggressive PCa using ZD2-Gd(HP-DO3A), compared with the
clinical control agent ProHance®. This contrast agent can
potentially facilitate accurate risk stratification and
clinical management of PCa.
|
| |
10:24
 |
0579.
 |
Short term Repeatability of Microstructural (VERDICT) MRI vs.
ADC in Prostate Cancer 
Edward William Johnston1, Eleftheria Panagiotaki2,
Elisenda Bonet-Carne2, Nicola Stevens1,
David Atkinson1, Daniel Alexander2,
and Shonit Punwani1
1UCL Centre for Medical Imaging, London, United
Kingdom, 2UCL
Centre for Medical Image Computing, London, United Kingdom
VERDICT (Vascular, Extracellular, and Restricted Diffusion
for Cytometry in Tumours) is a microstructural imaging
technique that has shown significant potential in
preclinical and pilot studies. However, its technical
repeatability is unknown and must be established for
translational and clinical application.
5 patients underwent consecutive VERDICT acquisitions,
and their quantitative parametric maps were compared in
tumour and non-tumour regions. We found that cellularity was
the most reliable parameter, with almost perfect
repeatability in both normal and cancerous prostate tissue.
Intra and extracellular volume fractions also performed
well, with almost perfect repeatability in the normal
prostate and excellent repeatability in cancerous tissue.
|
| |
10:36
|
0580.
 |
The Impact of Arterial Input Function Determination Variation on
Prostate Dynamic Contrast-Enhanced Magnetic Resonance Imaging
Pharmacokinetic Modeling: A Multicenter Data Analysis Challenge 
Wei Huang1, Yiyi Chen1, Andriy Fedorov2,
Xia Li3, Guido Jajamovich4, Dariya I
Malyarenko5, Madhava Aryal5, Peter S
LaViolette6, Matthew J Oborski7,
Finbarr O’Sullivan8, Richard G Abramson9,
Mark Muzi10, Kourosh Jafari-Khouzani 11,
Aneela Afzal1, Alina Tudorica1,
Brendan Moloney1, Cecilia Besa4,
Jayashree Kalpathy-Cramer11, James M Mountz7,
Charles M Laymon7, Kathleen Schmainda6,
Yue Cao5, Thomas L Chenevert5, Bachir
Taouli4, Thomas E Yankeelov9, Fiona
Fennessy2, and Xin Li1
1Oregon Health & Science University, Portland,
OR, United States, 2Brigham
and Women’s Hospital and Harvard Medical School, Boston, MA,
United States, 3General
Electric Global Research, Niskayuna, NY, United States, 4Icahn
School of Medicine at Mount Sinai, New York, NY, United
States, 5University
of Michigan, Ann Arbor, MI, United States, 6Medical
College of Wisconsin, Milwaukee, WI, United States,7University
of Pittsburgh, Pittsburg, PA, United States, 8University
College Cork, Cork, Ireland, 9Vanderbilt
University, Nashville, TN, United States, 10University
of Washington, Seattle, WA, United States,11Massachusetts
General Hospital and Harvard Medical School, Boston, MA,
United States
Dynamic Contrast-Enhanced MRI (DCE-MRI) pharmacokinetic
modeling is widely used to extract tissue specific
quantitative parameters. However, the accuracy and
precision of these parameters can be affected by many
factors, with arterial input function (AIF) determination
being a primary source of uncertainties. In this multicenter
study, we sought to evaluate variations in DCE-MRI
parameters estimated from shared prostate DCE-MRI data as a
result of differences in AIFs.
|
| |
10:48
|
0581.
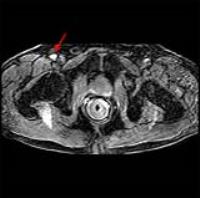 |
Using low dose prostate dynamic contrast enhanced MRI data to
verify newly developed eight-parameter mathematical form of
arterial input function - Permission Withheld
Xiaobing Fan1, Shiyang Wang1, Milica
Medved 1,
Tatjana Antic2, Serkan Guneyli 1,
Aytekin Oto 1,
and Gregory S Karczmar 1
1Radiology, University of Chicago, Chicago, IL,
United States, 2Pathology,
University of Chicago, Chicago, IL, United States
Accurate measurements of the arterial input function (AIF)
are needed in pharmacokinetic models to analyze dynamic
contrast enhanced (DCE) MRI data. The AIF often cannot be
accurately measured due to T2* and water exchange effects.
Therefore, population AIFs are often employed in
pharmacokinetic modeling. Here we report a new 8-parameter
empirical mathematical model (EMM) that fits the AIF
measured directly from the external femoral artery after a
dose of contrast agent that was greatly reduced to minimize
artifacts. The results showed that the EMM-AIF accurately
models both 1st and
2nd passes
of contrast agent circulations.
|
| |
11:00
|
0582.
 |
Quantitative DCE and DWI Characterization of the Index Lesion in
Multiparametric MRI of Prostate Cancer Patients 
Qing Yuan1, Daniel N Costa1,2, Julien
Sénégas3, Yin Xi1, Andrea J Wiethoff2,4,
Robert E Lenkinski1,2, and Ivan Pedrosa1,2
1Radiology, UT Southwestern Medical Center,
Dallas, TX, United States, 2Advanced
Imaging Research Center, UT Southwestern Medical Center,
Dallas, TX, United States, 3Philips
Research Laboratories, Hamburg, Germany, 4Philips
Research North America, Cambridge, MA, United States
We investigated the use of quantitative DWI and DCE
measurements in MRI-visible index lesions as a surrogate for
aggressiveness in prostate cancer patients. Tissue diffusion
coefficient from simplified intravoxel incoherent motion
model from DWI, and initial area under the curve from DCE
offered the best performance in discriminating low and
intermediate-to-high risk tumors. Anatomic and functional
multiparametric MRI may provide a more reliable assessment
of the aggressiveness of prostate cancer in patients.
|
| |
11:12
|
0583.
 |
Rad-Path correlation and machine learning generate epithelium
density maps predictive of pathologically confirmed prostate
cancer 
Amy L. Kaczmarowski1, Kenneth Iczkowski2,
William A. Hall3, Ahmad M. El-Arabi4,
Kenneth Jacobsohn4, Paul Knechtges1,
Mark Hohenwalter1, William See4, and
Peter S. LaViolette1
1Radiology, Medical College of Wisconsin,
Milwaukee, WI, United States, 2Pathology,
Medical College of Wisconsin, Milwaukee, WI, United States, 3Department
of Radiation Oncology, Medical College of Wisconsin,
Milwaukee, WI, United States, 4Urology,
Medical College of Wisconsin, Milwaukee, WI, United States
Radiological-pathological correlation is being used to
validate prostate cancer imaging technology. This study
combines these two modalities with machine learning to
generate predictive maps of histological features (i.e. new
contrasts) based on segmented histology. We find that
epithelium density maps highlight regions pathologically
confirmed as Gleason grade ≥3. This allowed the prediction
of prostate cancer presence based solely on non-invasive
imaging in 23 of 26 cases.
|
| |
11:24
|
0584.
 |
Quantitative MRI-Driven Deep Learning for Detection of Clinical
Significant Prostate Cancer 
Shiwen Shen1,2, Xinran Zhong1,3,
Willam Hsu1, Alex Bui1, Holden Wu1,
Michael Kuo1, Steven Raman1, Daniel
Margolis1, and Kyunghyun Sung1
1Department of Radiological Sciences, University
of California, Los Angeles, Los Angeles, CA, United States, 2Department
of Bioengineering, University of California, Los Angeles,
Los Angeles, CA, United States,3Physics and
Biology in Medicine IDP, University of California, Los
Angeles, Los Angeles, CA, United States
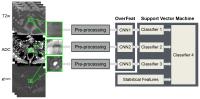
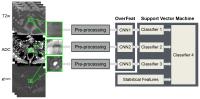
We present a novel automatic classification method to
distinguish between indolent and clinically significant
prostatic carcinoma using multi-parametric MRI (mp-MRI). The
main contributions are 1) utilizing state-of-art deep
learning method to characterize the lesion in mp-MRI through
a pre-trained convolutional neural network model, OverFeat, 2) building
a hybrid two-order classification model that combines deep
learning and conventional statistical features, and 3)
avoiding annotation of the lesion boundaries
and anatomical-location-specific training. The proposed
method was evaluated using 102 lesions of prostate cancer
and achieved significantly higher accuracy than the method
with traditional statistical features.
|
| |
11:36
|
0585.
 |
Dixon with view angle tilting for improved post-contrast MRI of
the prostate 
Silke Hey1, Vijayasarathy Elanchezhian2,
and Marius van Meel2
1Clinical Excellence & Research, Philips
HealthTech, Best, Netherlands, 2MR
Clinical Applications, Philips HealthTech, Best, Netherlands
A T1w TSE Dixon acquisition is combined with view angle
tilting (VAT) in order to reduce susceptibility induced
artifacts from orthopedic implants close to the prostate and
at the same time improve fat suppression in the area of
interest. The comparison with SPIR fat suppression shows
clear improvement when using Dixon together with VAT by
providing more homogeneous and complete fat suppression and
reduced susceptibility artifacts thus allowing clear
visualization of T1 based contrast changes in the prostate
and the surrounding tissue. Those results have been proven
at 1.5T and 3.0T on healthy volunteers with orthopedic hip
implants.
|
| |
11:48
 |
0586.
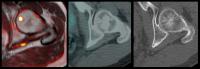 |
Multiparametric Whole-body MRI vs 18FCH-PET-CT in the Primary
Staging of Intermediate and High-Risk Prostate Cancer 
Edward William Johnston1, Arash Latifoltojar1,
Harbir Singh Sidhu1, Navin Ramachandran1,
Magdalena Sokolska2, Alan Bainbridge2,
Caroline Moore3, Hashim Ahmed3, and
Shonit Punwani1
1UCL Centre for Medical Imaging, London, United
Kingdom, 2Medical
Physics, University College London Hospital, London, United
Kingdom, 3Department
of Urology, University College Hospital, London, United
Kingdom
Whilst whole body MRI is gaining momentum in cancer staging
for multiple tumour types, relatively few groups have
focused on the primary staging of prostate cancer. In
this study, we evaluated the role of an extensive
multiparametric MRI protocol, including diffusion-weighted
imaging in 23 patients against an 18F-choline PET-CT/ expert
panel based reference standard.
According to the reference standard, we found that whole
body MRI provided an equivalently high diagnostic accuracy
vs. PET-CT in lymph nodes, and outperformed PET-CT in the
detection of bone lesions. However, higher technical error
rates suggest MRI reporting experience needs to be developed
first. |
|