Fetal & Placental MRI
Fetal & Placental MRI
Oral
Oral
Body: Breast, Chest, Abdomen, Pelvis
Thursday, 16 May 2019
| Room 516C-E | 08:15 - 10:15 | Moderators: Ashok Panigrahy, Daniela Prayer |
| 08:15 |
1070. 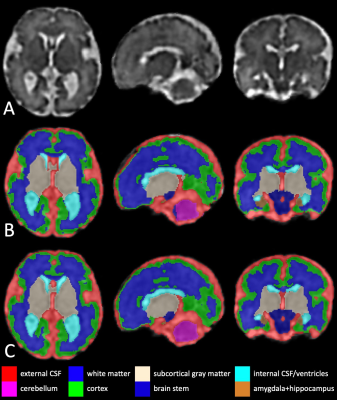 |
Fetal Brain Automatic Segmentation Using 3D Deep Convolutional Neural Network
Li Zhao, Xue Feng, Craig Meyer, Yao Wu, Adre du Plessis, Catherine Limperopoulos
Fetal brain MR image segmentation is necessary for brain development research. Currently, this task mainly relies on labor-intensive manually contouring or correction, because automatic segmentation often fails due to the low image quality. In this work, we apply a convolutional neural network, 3D U-Net, to segment the fetal brain regions. The proposed method was validated on 209 fetal brain MRI scans, including healthy fetal controls and high-risk fetuses with congenital heart disease. The proposed method showed high consistency with the manual correction results and may facilitate the identification of aberrant fetal brain development by providing quantitative morphological information.
|
08:27 |
1071. |
Quantifying T1 and T2* Relaxation Times of Fetal Fat, Fetal Liver, Fetal Kidney, and Amniotic Fluid at 1.5T
Simran Sethi, Stephanie Giza, Mary-Ellen Empey, Barbra de Vrijer, Charles McKenzie
T1 and T2* relaxation times of fetal tissues as a function of gestational age have not been previously published. We acquired fetal MRI data from pregnant women with a gestational age between 29 and 38 weeks. Using DESPOT1 and Quantitative IDEAL, the T1 and T2* relaxation times, respectively, of fetal fat, fetal liver, fetal kidney, and amniotic fluid were quantified as a function of gestational age. Only fetal fat T1 and T2* relaxation times, and fetal liver T2* relaxation times changed during this gestational period.
|
08:39 |
1072 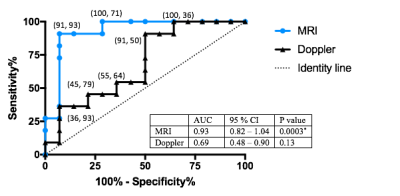 |
The Utility of MRI for Measuring Hematocrit in Fetal Anemia Video Permission Withheld
Jiawei Xu, An Qi Duan, Davide Marini, Johannes Keunen, Sharon Portnoy, John Sled, Brian McCrindle, John Kingdom, Christopher Macgowan, Mike Seed
To determine the accuracy of MRI for estimating hematocrit in anemic fetuses, the current study compared MRI-estimated hematocrit against the gold-standard fetal blood sampling and Doppler assessment of the middle cerebral artery for peak systolic velocity (MCA-PSV). MRI-estimated hematocrit was calculated from T1 and T2 measurements of intrahepatic umbilical vein blood. MRI results correlated well with fetal blood sampling and had a higher specificity for predicting anemia than Doppler MCA-PSV. In conclusion, MRI is feasible and accurate for the detection of fetal anemia and may be used to confirm the need for blood transfusion when MCA-PSV is suggestive of anemia.
|
| 08:51 |
1073. 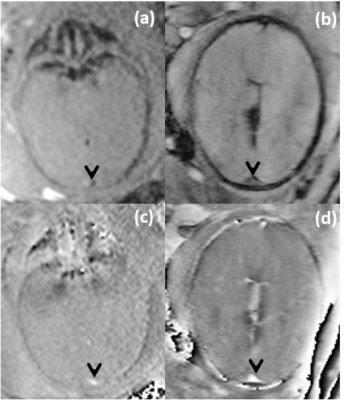 |
Dual-Imaging Modality Approach to Evaluate Cerebral Hemodynamics in Growth-Restricted Fetuses: Oxygenation and Perfusion
Brijesh Yadav, Edgar Andrade, Uday Krishnamurthy, Sagar Buch, Pavan Jella, Anabela Trifan, Lami Yeo, Sonia Hassan, E Haacke, Roberto Romero, Jaladhar Neelavalli
Cerebral blood perfusion has shown to be a sensitive biomarker of brain sparing at early stages of fetal growth restriction (FGR) compared to conventional Doppler estimates. Blood perfusion along with cerebral blood oxygenation may provide a holistic view of the fetal brain metabolism during FGR. Fractional moving blood volume, an ultrasound-based; and susceptibility weighted imaging, an MRI-based technique were used to estimate fetal cerebral blood perfusion and oxygenation, respectively. A significantly negative and positive correlation was found between cerebral blood perfusion and oxygenation, in normal growth and FGR fetuses, respectively. This dual modality based model will improve assessment of fetal well-being.
|
| 09:03 |
1074. 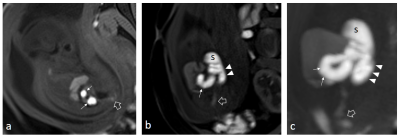 |
Using 3D Radial VIBE MR to Evaluate the Normal and Abnormal Gastrointestinal Tract in Fetuses
Taotao Sun, Ling Jiang, Zhongshuai Zhang, Mengxiao Liu, Marcel Nickel, Zhaoxia Qian
Images obtained with the radial VIBE sequence were reported to have less motion artifacts [MB1] than Cartesian sampled 3D VIBE T1W images in various pediatric regions. In this study, all cases with GI anomalies were diagnosed with acceptable image quality, including dilatation, narrowing, and herniation of the intestine. All parts of the colon were visualized and measurable after 24 weeks’ gestation. The results also indicate that an increasing trend of colon calibers with advancing gestational age, and a GA-specific caliber pattern that may improve the diagnosis of GI tract abnormalities. [MB1]There is no quantification & no image comparison proving this,
|
| 09:15 |
1075. 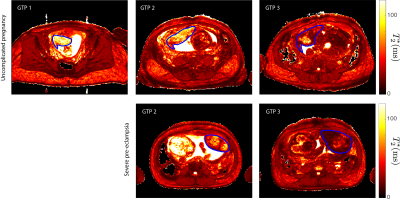 |
A Longitudinal Multisite Study of Endogenous BOLD MRI In Human Pregnancies
Matthias Schabel, Victoria Roberts, D. Rincon, Jessica Gaffney, Jamie Lo, Karen Gibbins, Nathan Blue, Glen Morrell, Christopher Kroenke, Robert Silver, Antonio Frias
The spatial distribution of placental T2* determined via BOLD MRI has been shown to correlate with maternal blood flow and corresponding blood oxygen levels within individual placental lobules. Here, we report data from a longitudinal multisite study aimed at assessing placental T2* across multiple gestational time points in human pregnancy and correlating it with pregnancy outcomes.
|
| 09:27 |
1076. 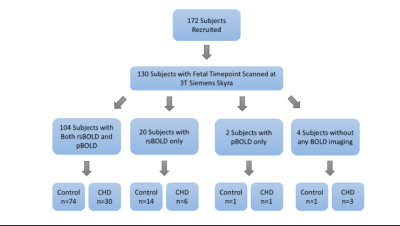 |
BOLD MR Imaging of Placenta in Congenital Heart Disease: Correlation with Maternal Risk Factors, Placental Pathology, and Maternal Serum Hormones
Alexander El-Ali, William Reynolds, Vidya Rajagopalan, Vincent Lee, Julia Wallace, Jenna Schabdach, Alexandra Zehner, Michelle Gruss, Jennifer Adibi, Vincent Schmithorst, Ashok Panigrahy
Intrinsic placental BOLD (pBOLD) was analyzed in mothers of congenital heart disease patients (CHD) and controls. The relationship between pBOLD temporal variance (primary outcome measure), CHD status and resting state fetal brain BOLD (rsBOLD) was specifically examined with secondary analyses exploring the relationship between pBOLD, placental histopathology, maternal risk factors (MRFs) and serum hormones (estriol, PAPP-A, β-hCG). We found that CHD patients demonstrated increased pBOLD temporal variance vs controls (p<0.001). When including the presence of MRFs (HTN, DM2, and Drug Use) as a covariate, a positive correlation between pBOLD and rsBOLD was identified (p=0.003).
|
| 09:39 |
1077. 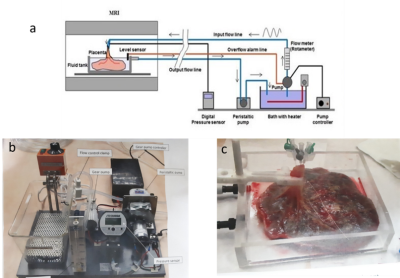 |
Studying human placental function ex-vivo using perfusion methods in MRI
Daphna Link, Oren Geri, Liat Ben Sira, Shaul Harel, Tuvia Genut, Zoya Gordon, Ariel Many, Dafna Ben Bashat
The aim of this study was to investigate the functional characteristics of the human placenta ex-vivo using a novel MR compatible perfusion system. Fifteen normal human placentas were scanned ex-vivo; bolus arrival time (BAT) and flow were extracted from TWIST data. Higher BAT and lower flow values were found in placentas with peripheral cord insertion. Significant correlations were obtained between BAT and the linear distance of the blood vessel from cord insertion location. This is the first work that studied the perfusion of human placentas with MRI and provides information regarding the relation between placental structure and function.
|
| 09:51 |
1078. 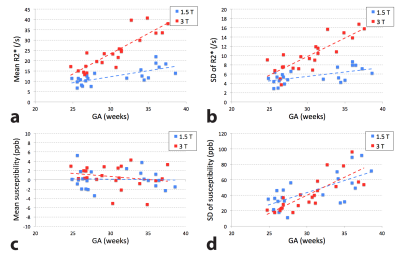 |
Feasibility of quantitative susceptibility mapping in the human placenta
Zungho Zun, Kushal Kapse, Jessica Quistorff, Alexis Gimovsky, Homa Ahmadzia, Nickie Andescavage, Catherine Limperopoulos
Quantitative susceptibility mapping (QSM) is an emerging tool for measuring magnetic susceptibility of tissue, which is used to identify hypoxia, hemorrhage, and calcifications. In this study we demonstrated the feasibility of performing QSM in the in-vivo human placenta. The measurement differences in R2* and susceptibility between 1.5 T and 3 T were consistent with our expectations and previous studies, and susceptibility was significantly reduced in response to maternal hyperoxia due to reduced deoxyhemoglobin. These results suggest that placental QSM may have the potential to assess placental function such as oxygenation.
|
| 10:03 |
1079. 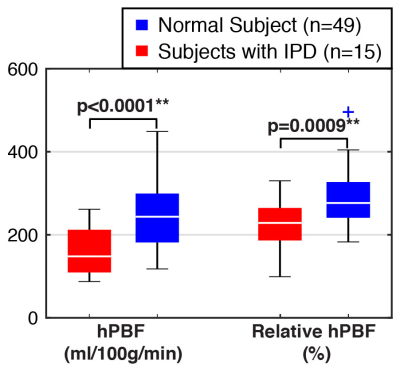 |
Prediction of Ischemic Placental Disease during Early Gestation using Pseudo-Continuous Arterial Spin Labeling MRI
KyungHyun Sung, Dapeng Liu, Xingfeng Shao, Alibek Danyalov, Teresa Chanlaw, Danny Wang, Carla Janzen, Sherin Devaskar
A real-time and non-invasive way to assess placental development would have great potential to help diagnose various conditions of placental insufficiency. Arterial spin labeling (ASL) MRI has great potential to serve as
|
 Back to Program-at-a-Glance |
Back to Program-at-a-Glance |  Back to Top
Back to Top