Scientific Session
Neurovascular Imaging
Session Topic: Neurovascular imaging
Session Sub-Topic: MRI in Diagnosis & Treatment of Cerebrovascular Diseases
Oral
Neuro
| Thursday Parallel 2 Live Q&A | Thursday, 13 August 2020, 14:20 - 15:05 UTC | Moderators: Anja van der Kolk |
Session Number: O-17
1052.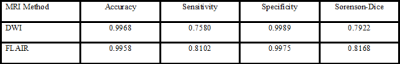 |
Comparison of Automated Cerebral Infarct Segmentation Techniques using DWI and FLAIR MRI
Ryan A. Rava1,2, Muhammad Waqas2,3, Kenneth V. Snyder2,3, Elad I. Levy2,3, Adnan H. Siddiqui2,3, Jason M. Davies2,3, Xiaoliang Zhang1, and Ciprian N. Ionita1,2,3
1Biomedical Engineering, University at Buffalo, Buffalo, NY, United States, 2Canon Stroke and Vascular Research Center, University at Buffalo, Buffalo, NY, United States, 3Neurosurgery, University at Buffalo, Buffalo, NY, United States
FLAIR MRI has the potential to provide more accurate ground truth infarct labels compared with DWI for the purpose of software validation and determination of ischemic stroke patient eligibility for thrombectomy. Currently, accurate segmentation of infarct has hindered the use of FLAIR infarct labels due to skull and erroneous image intensity values being similar to those of infarct lesions. In this study, an automated segmentation technique was developed for segmentation of infarct tissue from FLAIR MRI and performance metrics comparing this method to manually segmented infarct (FLAIR Sorenson-Dice=0.8168, DWI Sorenson-Dice=0.7922) indicate this technique is non-inferior to the current standard (DWI).
|
|
1053. |
FLAIR-based estimation of the stroke onset time: a magnetic field dependent study
Tao Jin1
1Department of Radiology, University of Pittsburgh, Pittsburgh, PA, United States
Stroke onset time is a prerequisite for thrombolytic treatment but is unknown in ~25% of acute ischemic stroke patients. A fluid-attenuated inversion recovery (FLAIR)-based MRI index (e.g., DWI-FLAIR mismatch) has been suggested as a surrogate to determine whether the stroke duration is within the treatment window. In this work, we showed that the time when a positive FLAIR contrast appears between ischemic and normal tissue increases with B0, and is dependent on the imaging parameters. Therefore, FLAIR-based studies of stroke onset should be designed or interpreted with care.
|
|
1054.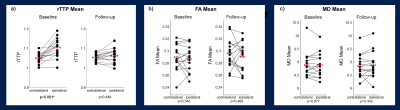 |
Stable fractional anisotropy and mean diffusivity after treatment in patients with asymptomatic high grade internal carotid artery stenosis
Lena Schmitzer1, Stephan Kaczmarz1,2, Nico Sollmann1, Claus Zimmer1, Christine Preibisch1,3, and Jens Göttler1,2,4
Video Permission Withheld
1School of Medicine, Department of Neuroradiology, Technical University of Munich, Munich, Germany, 2MRRC, Yale University, New Haven, CT, United States, 3School of Medicine, Clinic of Neurology, Technical University of Munich, Munich, Germany, 4School of Medicine, Department of Radiology, Technical University of Munich, Munich, Germany
Internal carotid artery stenosis (ICAS) is a well-known risk factor for stroke. However, treatment efficacy evaluations are currently limited by widely unknown ICAS-effects on brain microstructure. Two promising parameters to study pathophysiological changes in white matter (WM) are fractional anisotropy (FA) and mean diffusivity (MD), derived from established diffusion-tensor imaging. We evaluated FA- and MD-maps in 15 ICAS-patients before and after revascularization. Our results demonstrated globally unimpaired FA and MD before treatment, even in watershed areas, which are especially vulnerable to hemodynamic impairments. Postinterventional structural results were stable. Thus, absence of ischemic events and successful treatment are indicated.
|
|
1055.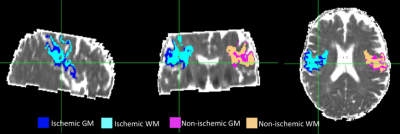 |
Determining stroke onset time using T2 relaxation times: A comparison of reference and reference independent methods in ischemic stroke patients
Bryony L. McGarry1, Robin A. Damion1, Terence J. Norton1, Michael J. Knight1, Philip L. Clatworthy2, George W.J. Harston3, Keith W. Muir4, and Risto A. Kauppinen5
1School of Psychological Science, University of Bristol, Bristol, United Kingdom, 2Stroke Neurology, North Bristol NHS Trust, Bristol, United Kingdom, 3Acute Stroke Programme, Radcliffe Department of Medicine, University of Oxford, Oxford, United Kingdom, 4Institute of Neuroscience and Psychology, University of Glasgow, Glasgow, United Kingdom, 5Faculty of Engineering, University of Bristol, Bristol, United Kingdom
Unknown onset time is a common contradiction for anti-thrombolytic treatment of ischemic stroke. T2 relaxation times within the lesion estimate onset time, but accuracy may be affected by dependence on the non-ischemic hemisphere as reference for pre-ischemic values. In hyperacute ischemic stroke patients, we tested a reference-independent approach shown to be an accurate timer in a preclinical stroke model. This involved modelling the T2 distribution within ADC defined lesions to design linear regression models for onset time estimation. The reference-independent approach was accurate in grey matter and for lesions containing grey and white matter, the reference-dependent approach was more accurate.
|
|
 |
1056.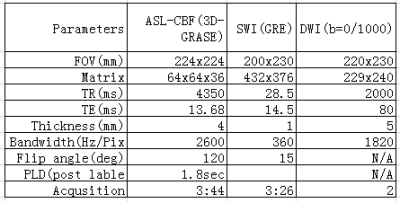 |
A Comparative Analysis of CEST-APT, SWI-QSM, DWI and ASL-CBF in Ischemic Stroke Patients
Guomin Li1, Hui Liu2, Qi Liu2, Yongquan Ye2, Yichen Hu2, Haodong Qin3, Jun Xie3, Jianhao Yan4, Yang Xin3, and Guihua Jiang4
1Medical Imaging, Guangdong Second Provincial General Hospital, Guangzhou, China, 2UIH America, Inc., Houston, TX, United States, 3United Imaging Healthcare, Shanghai, China, 4Guangdong Second Provincial General Hospital, Guangzhou, China
In this study, APT, SWI-QSM, ASL-CBF, and DWI imaging are compared and evaluated in stroke patients, with a focus on different values in identifying diseased area and helping to provide better prognosis.
|
1057.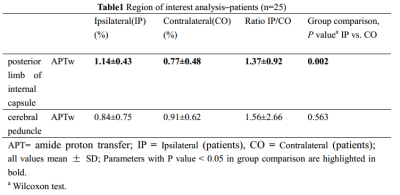 |
Amide Proton Transfer Magnetic Resonance Imaging detecting early Wallerian degeneration of the pyramidal tract after ischemic stroke
Junxin Wang1, Yanwei Miao1, Jiazheng Wang2, Zhiwei Shen2, Bingbing Gao1, Yu Bing1, Yunan Cui1, Ailian Liu1, and Qingwei Song1
1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Phillips healthcare, China, China
The study aimed to evaluate the significance of amide proton transfer weighted (APTw) imaging in the early diagnosis of pyramidal tract Wallerian degeneration (WD) following cerebral infarction. This study included 25 patients with acute cerebral infarction and 12 healthy adult controls. Our data suggested that the value of APTw was significantly increased on ipsilateral compared to contralateral and the control group in the posterior limb of internal capsule. It proves the feasibility of APTw in early detection of WD.
|
|
1058.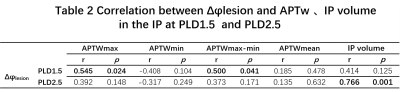 |
Correlation between APTw changes and regional cerebral oxygen metabolism in ischemic tissue of patients with subacute ischemic stroke
Yuhan Jiang1, Yanwei Miao1, Peipei Chang1, Zhongping Zhang2, Yiwei Che1, Ailian Liu1, Qingwei Song1, and Jiazheng Wang2
1the First Affiliated Hospital of Dalian Medical University, Dalian, China, Dalian, China, 2Philips Healthcare, Beijing, China, Beijing, China
The relationship between APTw and regional cerebral oxygen metabolism levels in the ischemic area is unclear. This study attempts to investigate the mechanism of ischemic tissue pH changes and its influencing factors by measuring the APTw value of ischemic tissue, combined with ASL and SWI. We found that the phase differences of the veins in the infarct (Δφlesion) is positively correlated with APTWmax and APTWmax-min in the ischemic penumbra at PLD1.5.
|
|
 |
1059.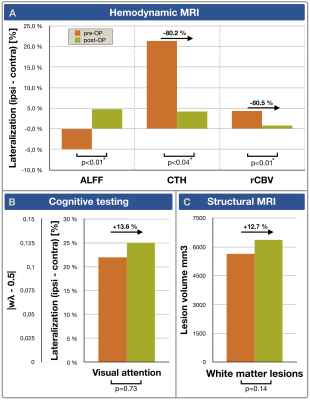 |
Treatment efficacy of asymptomatic carotid artery stenosis patients evaluated by clinically applicable hemodynamic MRI and cognitive testing
Stephan Kaczmarz1,2, Jens Göttler1,2,3, Jan Petr4, Nico Sollmann1, Lena Schmitzer1, Andreas Hock5, Mikkel Bo Hansen6, Kim Mouridsen6, Claus Zimmer1, Fahmeed Hyder2, and Christine Preibisch1,7
1School of Medicine, Department of Neuroradiology, Technical University of Munich, Munich, Germany, 2MRRC, Yale University, New Haven, CT, United States, 3School of Medicine, Department of Radiology, Technical University of Munich, Munich, Germany, 4Institute of Radiopharmaceutical Cancer Research, Helmholtz-Zentrum Dresden-Rossendorf, Dresden, Germany, 5Philips Healthcare, Hamburg, Germany, 6Institute of Clinical Medicine, Aarhus University, Aarhus, Denmark, 7School of Medicine, Clinic of Neurology, Technical University of Munich, Munich, Germany
Hemodynamic MRI is highly promising to improve treatment decisions in asymptomatic internal carotid artery stenosis (ICAS). However, treatment efficacy evaluations require clinically applicable techniques, such as dynamic susceptibility contrast (DSC) and resting-state BOLD-based evaluations of amplitude of low-frequency fluctuations (ALFF). We present data from 16 asymptomatic ICAS patients before and after treatment and 17 age-matched healthy controls measuring cerebral blood volume (CBV) and capillary transit-time heterogeneity (CTH) by DSC and ALFF with additional cognitive testing. We hypothesized recovery of hemodynamic impairments after revascularization. Our results confirmed this hypothesis for all parameters. Interestingly, at the same time cognitive function remained impaired.
|
1060.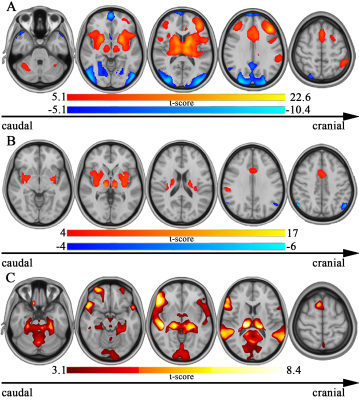 |
Network mapping of central post-stroke pain and analgesic neuromodulation
Gavin J B Elias1, Philippe De Vloo2, Jürgen Germann1, Alexandre Boutet1, Robert M Gramer1, Suresh E Joel3, Bart Morlion2, Bart Nuttin2, and Andres M Lozano1
1University Health Network, Toronto, ON, Canada, 2University Hospitals Leuven, Leuven, Belgium, 3GE Global Research, Bangalore, India
Despite the prevalence of central post-stroke pain (CPSP), pain-causing brain lesions remain incompletely understood. In 17 CPSP patients receiving invasive neuromodulation, we utilized voxelwise odds-ratio mapping and normative resting state fMRI to identify high-risk pain hotspots and describe functional networks associated with CPSP lesions and analgesic stimulation. Highest-risk CPSP hotspots were located in somatosensory thalamus/white matter and connected to a network comprising anterior cingulate cortex, insula, thalamus, and inferior parietal lobule. Posterior insula and thalamus were also coupled to therapeutic deep brain stimulation volumes. These findings elucidate CPSP’s topography and connectivity while informing the network-level mechanism of analgesic neuromodulation.
|

 Back to Program-at-a-Glance
Back to Program-at-a-Glance Watch the Video
Watch the Video Back to Top
Back to Top