Scientific Session
Thoracic/Lung MRI
Session Topic: Thoracic/Lung MRI
Session Sub-Topic: Thoracic MRI
Oral
Body
| Tuesday Parallel 3 Live Q&A | Tuesday, 11 August 2020, 13:45 - 14:30 UTC | Moderators: Bastiaan Driehuys |
Session Number: O-24
 |
0427.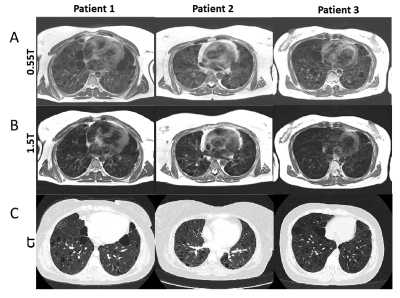 |
Structural and functional lung imaging using a high performance 0.55T MRI system
Ipshita Bhattacharya1, Rajiv Ramasawmy1, Joel Moss1, Marcus Y Chen1, Waqas Majeed2, Thomas Benkert3, Robert S Balaban1, and Adrienne Campbell-Washburn1
1National Institutes of Health, Bethesda, MD, United States, 2Siemens Medical Solutions, Malvern, PA, United States, 3Siemens Healthcare GmbH, Erlangen, Germany
Lung imaging using conventional MRI has several limitations for clinical use. A contemporary low-field MRI (0.55T) system offers several advantages for structural and functional imaging of lung owing to low magnetic susceptibility and increased oxygen relaxivity. In this abstract we present an improved structural imaging method and functional imaging method for patients with lymphangioleiomyomatosis (LAM) at low-field. Anatomical imaging offers improved delineation of cystic structures in the lung parenchyma. Oxygen-enhanced lung MRI is used to measure ventilation and regional texture in healthy volunteers and this patient group with abnormal pulmonary function.
|
 |
0428.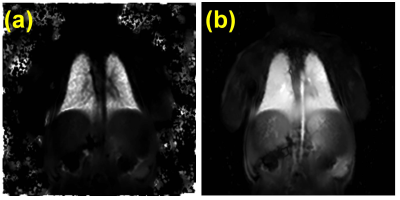 |
Feasibility of Structural and Phase-Resolved Functional Lung (PREFUL) MRI in Free-Breathing Neonates
Brandon Zanette1, Samal Munidasa1,2, Marcus J Couch1, Elaine Stirrat1, Eric Schrauben1, Robert Grimm3, Andreas Voskrebenzev4,5, Jens Vogel-Claussen4,5, Ravi Seethamraju6, Christopher K Macgowan1,2, Mary-Louise C Greer7,8, Emily Tam9,10, and Giles Santyr1,2
1Translational Medicine, The Hospital for Sick Children, Toronto, ON, Canada, 2Medical Biophysics, University of Toronto, Toronto, ON, Canada, 3MR Predevelopment, Siemens Healthcare, Erlangen, Germany, 4Diagnostic and Intervetional Radiology, Hannover Medical School, Hannover, Germany, 5Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), Member of the German Center for Lung Research (DZL), Hannover, Germany, 6MR Collaborations North East, Siemens Healthineers, Boston, MA, United States, 7Diagnostic Imaging, The Hospital for Sick Children, Toronto, ON, Canada, 8Medical Imaging, University of Toronto, Toronto, ON, Canada, 9Neurosciences and Mental Health, The Hospital for Sick Children, Toronto, ON, Canada, 10Neurology, The Hospital for Sick Children, Toronto, ON, Canada
MRI of the neonatal pulmonary system can be a useful tool for the clinical evaluation of lung structure and function without ionizing radiation. Despite this, the inherent challenges associated with MRI of the lung make this difficult. This works demonstrates the feasibility of structural and functional imaging of the neonatal lung without exogenous contrast using a clinical whole-body 3T system with standard coils in neonates without any cardiorespiratory history. The imaging protocol includes T1-weighted, T2-weighted, and ultrashort echo time (UTE) imaging for structural imaging as well as novel free-breathing Phase-Resolved Function Lung (PREFUL) MRI for ventilation/perfusion imaging.
|
0429.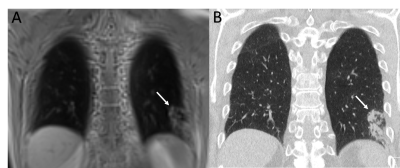 |
Non-contrast-enhanced 3D-UTE MRI for pulmonary Imaging of Immunocompromised Patients during Hematopoietic Stem Cell Transplantation
Corona Metz1, David Böckle2, Julius Frederik Heidenreich1, Andreas Max Weng 1, Thomas Benkert3, Götz Ulrich Grigoleit2, Herbert Köstler1, Thorsten Alexander Bley1, and Simon Veldhoen1
1Department of Diagnostic and Interventional Radiology, University Hospital Würzburg, Würzburg, Germany, 2Department of Internal Medicine II, University Hospital Würzburg, Würzburg, Germany, 3Application Development, Siemens Healthcare GmbH, Erlangen, Germany
Immunocompromised patients during HSCT procedure commonly need repeated MDCT examinations resulting in a high cumulative radiation dose. 3D-UTE MRI using a stack-of-spirals trajectory, enables contrast-free and radiation-free imaging of the lungs within a single breath-hold with increased signal yield due to echo times being well below parenchymal T2*. 3D-UTE MRI allows diagnostics of inflammatory consolidations and pleural effusions with high sensitivity, specificity and consistency when compared to MDCT. Moreover, 3D-UTE sequences improve detection rates of ground glass opacities in pulmonary MRI.
|
|
 |
0430.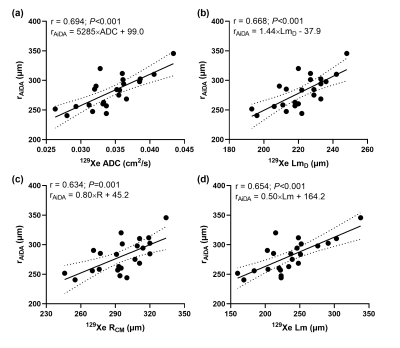 |
Benchmarking acinar airway measurements from inhaled nanoparticles with hyperpolarized 129Xe diffusion-weighted MRI
Ho-Fung Chan1, Madeleine Petersson Sjögren2, Paul J.C. Hughes1, Oliver I Rodgers1, Guilhem J Collier1, Graham Norquay1, Lars E Olsson3, Per Wollmer3, Jakob Löndahl2, and Jim M Wild1
1Academic Radiology, University of Sheffield, Sheffield, United Kingdom, 2Division of Ergonomics and Aerosol Technology, Lund University, Lund, Sweden, 3Department of Translational Medicine, Lund University, Malmö, Sweden
Airspace Dimension Assessment with inhaled nanoparticles (AiDA) and hyperpolarized 129Xe diffusion-weighted (DW)-MRI was performed in twenty-three healthy volunteers to benchmark measurements from AiDA against those from 129Xe DW-MRI. Significant correlations were observed between AiDA derived root mean square distal airspace radius, and 129Xe apparent diffusion coefficient and diffusion model derived acinar airway dimensions. Furthermore, the AiDA recovery at zero-second breath-hold significantly correlated with 129Xe alpha index from the stretched exponential model, a marker of acinar airspace heterogeneity. This benchmarking study demonstrates the potential of AiDA as an alternative method for the clinical evaluation of acinar airway microstructure changes.
|
 |
0431.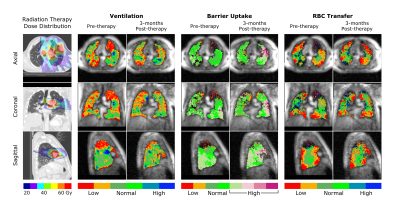 |
Quantitative dose-dependent changes in regional lung function after radiation therapy detected using xenon-129 gas exchange MRI
Leith Rankine1,2, Ziyi Wang1, Elianna Bier1, Christopher Kelsey3, Shiva Das2, Lawrence Marks2, and Bastiaan Driehuys1
1Center for In Vivo Microscopy, Duke University, Durham, NC, United States, 2Department of Radiation Oncology, University of North Carolina, Chapel Hill, NC, United States, 3Department of Radiation Oncology, Duke University Medical Center, Durham, NC, United States
Radiation therapy (RT) is widely used to treat lung cancer, but damage to surrounding healthy tissues can lead to compromised lung function. In this study, patients undergoing RT were imaged pre- and post-treatment using hyperpolarized 129Xe gas exchange MRI to assess for RT-induced changes in regional lung function. At 3-months post-treatment, a dose-response was evident in ventilation and gas exchange. Lung regions receiving ≥20Gy exhibited significantly increased barrier uptake and decreased RBC transfer. This may help radiation oncologists further understand the dose-dependence of RT-induced lung injury, and design dose distributions with fewer treatment toxicities.
|
 |
0432.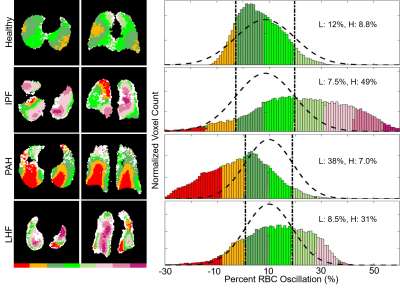 |
Imaging Regional Capillary Cardio-Pulmonary Blood Flow Dynamics using Hyperpolarized 129Xe MRI and Keyhole Reconstruction
Peter James Niedbalski1, Elianna A Bier2,3, Ziyi Wang2,3, Matthew M Willmering1, Bastiaan Driehuys2,3,4, and Zackary I Cleveland1,5
1Center for Pulmonary Imaging Research, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 2Department of Biomedical Engineering, Duke University, Durham, NC, United States, 3Center for In Vivo Microscopy, Duke University Medical Center, Durham, NC, United States, 4Department of Radiology, Duke University Medical Center, Durham, NC, United States, 5Department of Pediatrics, University of Cincinnati Medical Center, Cincinnati, OH, United States
Hyperpolarized 129Xe MRI offers the ability to analyze pulmonary gas transfer by imaging 129Xe dissolved in red blood cells (RBCs) separately from 129Xe in other tissues. A notable feature of the dissolved 129Xe signal is the presence of small cardiogenic oscillations in the 129Xe RBC signal, which have been used to characterized global abnormalities in pulmonary microvascular hemodynamics. Here, we demonstrate that these cardiogenic oscillations can be mapped 3-dimensionally to image capillary bed hemodynamics. Our approach uses keyhole reconstruction of standard 129Xe gas exchange MR acquisitions. Metrics obtained from these maps distinguished healthy from disease cohorts and predicted disease progression.
|
0433.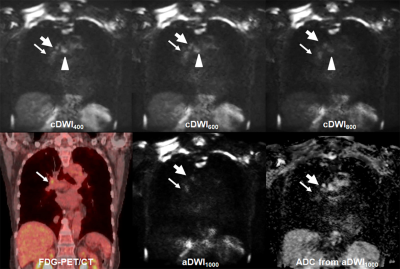 |
Computed Diffusion-Weighted Imaging in the Thorax: Determination of Appropriate b Value for Improving N-Stage Assessment in NSCLC Patients
Yoshiharu Ohno1,2, Masao Yui3, Daisuke Takenaka4, Yoshimori Kassai3, Kazuhiro Murayama1, and Takeshi Yoshikawa2
1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan
No major papers that determined the utility of cDWI for diagnosis of lymph node metastasis have been reported. We hypothesize that cDWI has a potential for improving diagnostic performance of N-stage in NSCLC patients as compared with aDWI and FDG-PET/CT, when set appropriate b value. The purpose of this study is to determine the utility of cDWI for differentiating metastatic from non-metastatic lymph nodes in NSCLC patients as compared with aDWI and FDG-PET/CT.
|
|
0434.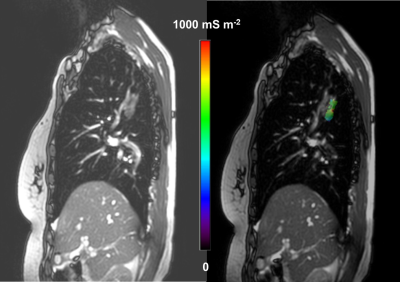 |
Noninvasive Assessment of Electrical Conductivity of Lung and Mediastinal Mass Lesions: Feasibility and Potential Clinical Value
Khin Khin Tha1,2, Ulrich Katscher3, Eiki Kikuchi4, Yasuka Kikuchi1, Yuki Yoshino1, Kinya Ishizaka5, Noriko Manabe1,2, Kohsuke Kudo1,2, and Hiroki Shirato2
1Department of Diagnostic and Interventional Radiology, Hokkaido University Hospital, Sapporo, Japan, 2Global Station for Quantum Medical Science and Engineering, Hokkaido University, Sapporo, Japan, 3Philips Research Laboratories, Hamburg, Germany, 4First Department of Medicine, Hokkaido University Hospital, Sapporo, Japan, 5Department of Radiological Technology, Hokkaido University Hospital, Sapporo, Japan
We evaluated the feasibility of σ measurable by EPT in evaluating lung and mediastinal mass lesions. EPT was performed in 21 patients with lung or mediastinal mass lesions. The lesion σ distribution, its relationship with histological findings, lesion size, location and the number of successful scans were evaluated. The malignant tumors had larger maximum σ and intralesional standard deviation and contrast. The larger the lesions, the greater were the intralesional contrast and entropy. The number of possible dynamic scans for reconstruction appeared to be larger in the upper lobe tumors, but the findings need to be confirmed with larger samples.
|
|
0435.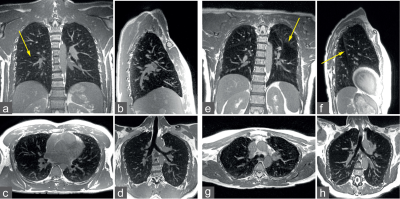 |
Thoracic imaging using balanced steady-state free precession with half-radial dual-echo readout (bSTAR)
Grzegorz Bauman1,2 and Oliver Bieri1,2
1Radiological Physics, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Allschwil, Switzerland
This work demonstrates the application of single-breathold thoracic MRI with balanced steaty-state free precession half-radial dual-echo readout technique (bSTAR) in human subjects. The proposed imaging technique combines a minimal-TR acquisition with a smoothly interleaved Archimedean spiral trajectory, which results in markedly improved signal intensity from low proton lung parenchyma tissue, improved visualization of the pulmonary vascular tree as well as a successful mitigation of eddy current and cardiac motion artifacts.
|
|
 |
0436.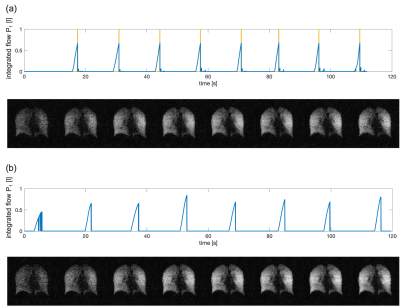 |
Volume-controlled 19F MR imaging of fluorinated gas wash-in
Arnd Jonathan Obert1,2, Marcel Gutberlet1,2, Agilo Luitger Kern1,2, Frank Wacker1,2, and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany
Since Perfluoropropane is highly inert, and can be mixed with oxygen, patients can inhale up to 30 liters of gas during one examination without a significant physiological impact. This enables detailed measurements of gas wash-in dynamics using 19F magnetic resonance imaging. In this work, an experimental setup for volume-controlled imaging of multiple breath-holds is realized using a pneumotachometer and pneumatic valves as well as MR triggering. In three healthy volunteers, the stability of the breathing volumes and the positions of the diaphragm, as well as the standard deviation of wash-in times, were analyzed comparing volume-controlled to non-controlled scans.
|

 Back to Program-at-a-Glance
Back to Program-at-a-Glance Watch the Video
Watch the Video Back to Top
Back to Top