Oral - Power Pitch Session
Pediatric Innovations
| Monday Parallel 3 Live Q&A | Monday, 10 August 2020, 13:45 - 14:30 UTC | Moderators: Wilburn Reddick |
 |
0076.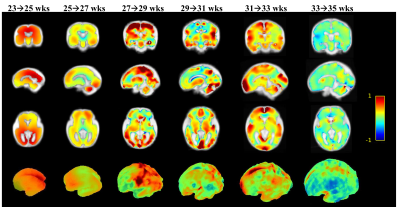 |
Mapping fetal brain development based on automated brain segmentation and 4D brain atlasing
Haotian Li1, Guohui Yan2, Wanrong Luo1, Tingting Liu1, Yan Wang1, Yi Zhang1, Li Zhao3, Catherine Limperopoulos3, Yu Zou2, and Dan Wu1
1Key Laboratory for Biomedical Engineering of Ministry of Education, Department of Biomedical Engineering, College of Biomedical Engineering & Instrument Science, Zhejiang University, Hangzhou, Zhejiang, China, 2Department of Radiology, Women's Hospital,School of Medicine,Zhejiang University, Hangzhou, Zhejiang, China, 3Diagnostic Imaging and Radiology, Children's National Medical Center, Washington, DC, WA, United States
Fetal brain MRI has become an important tool for in-utero assessment of brain development and disorders. Here we proposed an automated pipeline with fetal brain segmentation, super-resolution reconstruction, and fetal brain atlasing to quantitatively map in-utero fetal brain development in a Chinese population. We designed a U-net CNN implemented for automatic fetal brain segmentation, which showed superior segmentation accuracy compared with conventional methods. We then generated a Chinese fetal brain atlas, using an iterative linear and nonlinear registration method. Based on the 4D spatiotemporal atlas, we characterized the three-dimensional morphological evolution of the fetal brain between 23-36 weeks of gestation.
|
 |
0077.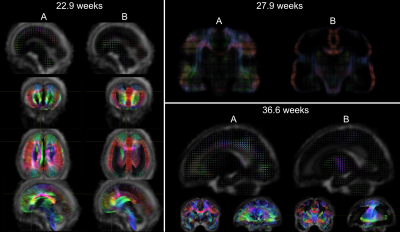 |
Multi-component atlas of fetal brain development via decomposition of diffusion MRI
Maximilian Pietsch1,2, Daan Christiaens2,3, Jana Hutter1,2, Lucilio Cordero-Grande1,2, Anthony N. Price1,2, Emer Hughes2, David Edwards2, Joseph V. Hajnal1,2, Serena J. Counsell2, and J-Donald Tournier1,2
1Biomedical Engineering Department, School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2Centre for the Developing Brain, School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 3Department of Electrical Engineering (ESAT/PSI), KU Leuven, Leuven, Belgium
Mapping tissue maturation in the fetal brain with diffusion MRI requires modelling transient processes in early brain development. In this work, we extend a data-driven multi-component framework introduced for modelling neonatal brain development to fetal data of the developing Human Connectome Project (dHCP). To this end, we build weekly templates ranging from 23 to 37 weeks gestational age that consist of one fluid and two orientationally-resolved tissue components. The orientation-resolved components exhibit marked spatial patterns and temporal trajectories, and demonstrate pronounced microstructural changes with gestational age.
|
0078.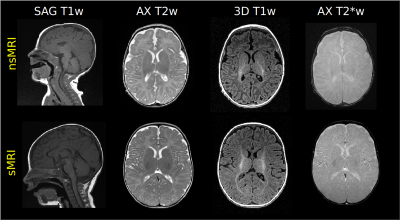 |
Evaluation of brain MRI quality in natural sleep vs anaesthesia in infants within 6 months of life.
Paolo Bosco1, Simona Fiori2, Rosa Pasquariello1, Elena Scaffei2,3, Michela Tosetti1, and Laura Biagi1
1Laboratory of Medical Physics and Magnetic Resonance, IRCCS Stella Maris Foundation, Pisa, Italy, 2Department of Developmental Neuroscience, IRCCS Stella Maris Foundation, Pisa, Italy, 3Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Natural sleep brain MRI (nsMRI) up to 6 months of life to support early diagnosis in term and preterm infants at high risk for cerebral palsy and other developmental disorders is still far from clinical practice, due to unproven feasibility and quality. We extracted some measures of quality (signal to noise ratio, contrast to noise ratio in a cohort of 23 and 53 infants who underwent sedation or natural sleep brain MR respectively. Most of the quality measures extracted across different MR modalities did not differ between nsMRI and sedation MRI (sMRI) suggesting the feasibility of nsMRI at younger ages.
|
|
0079.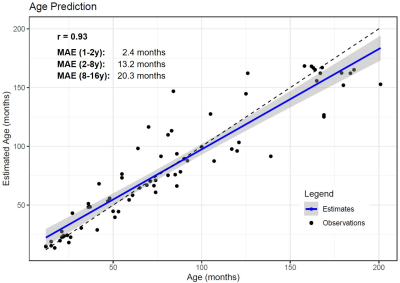 |
Measuring brain maturation with quantitative MRI
Gian Franco Piredda1,2,3, Tom Hilbert1,2,3, Baptiste Morel4,5, Clovis Tauber4, Jean Philippe Cottier4, Lars Lauer6, Jean-Philippe Thiran2,3, Bénédicte Maréchal1,2,3, and Tobias Kober1,2,3
1Advanced Clinical Imaging Technology, Siemens Healthcare AG, Lausanne, Switzerland, 2Department of Radiology, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland, 3LTS5, École Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland, 4UMR 1253, iBrain, Université de Tours, Inserm, Tours, France, 5Pediatric Radiology Department, Clocheville Hospital, CHRU of Tours, Tours, France, 6SHS DI MR SIP, Siemens Healthcare GmbH, Erlangen, Germany
The sensitivity of T1 mapping towards brain maturation during the first years of life was shown in previous studies. This work investigates whether this sensitivity is high enough that age of young subjects can be directly estimate from T1 relaxometry, which in turn enables to determine the developmental stage of the subject’s brain. A random forest regression was employed to estimate subjects’ age based on median T1 values of different brain regions. Good correlation (r=0.95) was found between actual and predicted ages, and proof-of-concept results in a patient showed the potential of the proposed framework to detect developmental delays.
|
|
 |
0080.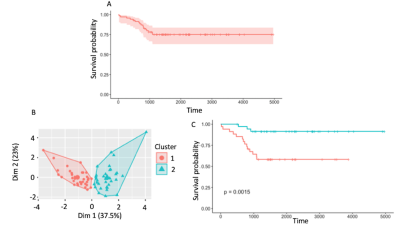 |
Deriving survival risk features using multi-parametric MRI in paediatric neuro-oncological disease: a multi-centre clinical study.
James Timothy Grist1, Stephanie Timothy Withey1, Lesley MacPherson2, Adam Oates3, Stephen Timothy Powell1, Jan Novak4, Laurence Abernethy5, Barry Pizer6, Ricahrd Grundy7, Simon Bailey8, Dipayan Mitra8, Theodoros N Arvantis9, Dorothee P. Auer7,
and Andrew C Peet1
1University of Birmingham, Birmingham, United Kingdom, 2Birmingham Women's and CHildren's NHS foundation trust, Birmingham, United Kingdom, 3Birmingham Women's and Children's NHS foundation trust, Birmingham, United Kingdom, 4Aston University, Birmingham, United Kingdom, 5Alder Hey Children's NHS foundation trust, Liverpool, United Kingdom, 6Institute of Translation Medicine, University of Liverpool, Liverpool, United Kingdom, 7University of Nottingham, Nottingham, United Kingdom, 8Royal Victoria Infirmary, Newcastle, United Kingdom, 9University of Warwick, Warwick, United Kingdom
This study focuses on the combination of diffusion and perfusion imaging with advanced machine learning to predict survival in a cohort of paediatric brain tumours. Results show two novel subgroups with significantly different survival. These results will aid in clinical decision making and therapeutic studies.
|
 |
0081.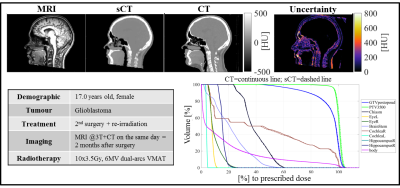 |
Deep learning-based sCTs with uncertainty estimation from heterogeneous paediatric brain MRI
Matteo Maspero1,2, Laura G Bentvelzen1,2, Mark H F Savenije1,2, Enrica Seravalli1, Geert O R Janssens1,3, Cornelis A T van den Berg1,2, and Marielle E P Philippens1
1Radiotherapy, UMC Utrecht, Utrecht, Netherlands, 2Computational imaging group for MR diagnostic & therapy, UMC Utrecht, Utrecht, Netherlands, 3Paediatric Oncology, Princess Maxima Center, Utrecht, Netherlands
The feasibility of radiotherapy dose calculations for brain tumours from MRI acquired with a heterogeneous set of acquisition protocols on paediatric patients was investigated using a combination of networks trained on orthogonal planes to estimate the uncertainty of the generated sCT.
|
 |
0082. |
Disrupted structural connectome in Duchenne’s muscular dystrophy: Classifying and subtyping based on Dp140 dystrophin isoform
Apurva Shah1, Apoorva Safai1, Veeramani Preethish Kumar2, Atchayaram Nalini2, Jitender Saini3, and Madhura Ingalhalikar1
1Symbiosis Center for Medical Image Analysis, Symbiosis International University, Pune, India, 2Department of Neurology, National Institute of Mental Health and Neurosciences, Bengaluru, India, 3Department of Radiology, National Institute of Mental Health and Neurosciences, Bengaluru, India
Duchenne Muscular Dystrophy (DMD) is a genetic neuromuscular disorder, characterized by muscle weakness and cognitive deficits due to mutation in DMD gene. Dp140+ and Dp140- are DMD subtypes derived based on promoter site of isoform Dp140 in DMD gene. Our work investigated the structural connectivity in DMD and its sub-types and demonstrated widespread and global reduction in connectivity across whole brain in DMD compared to controls. Higher dysconnectivity was observed in Dp140- subtype especially in cerebellar and frontal regions compared to Dp140+ implying that the promotor site of Dp140 isoform plays a crucial role in terms of impaired information processing.
|
0083.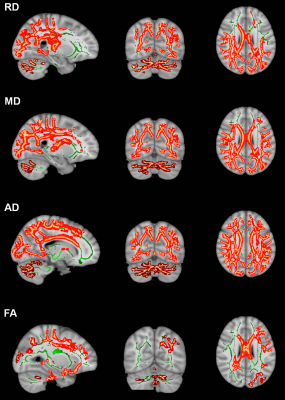 |
In vivo evaluation of white matter abnormalities in children with DMD using diffusion MRI
Jitender Saini1, Veeramani Preethish Kumar2, Apurva Shah3, Manoj Kumar4, Madhura Ingalhalikar5, and Nalini Atchayaram 2
1Nueroimaging and Interventional Radiology, National Institute of Mental Health and, Bangalore, India, 2Neurology, National Institute of Mental Health and, Bangalore, India, 33Symbiosis Centre for Medical Image Analysis, Symbiosis International University, Pune, India, 4Neuroimaging and Interventional Radiology, National Institute of Mental Health and, Bangalore, India, 5Symbiosis Centre for Medical Image Analysis, Symbiosis International University, Pune, India
Duchenne muscular dystrophy (DMD), a genetically inherited X-linked neuromuscular disorder characterised by progressive muscle weakness and significant non-motor manifestations like poor IQ, and neuropsychiatric illnesses. In this study, we evaluate white matter (WM) abnormalities in DMD patients using diffusion tensor imaging (DTI). We observed widespread WM changes in DMD patients and the presence of distal mutation was associated with poor clinical and neuropsychological profile with severe and spatially more WM abnormalities.
|
|
 |
0084.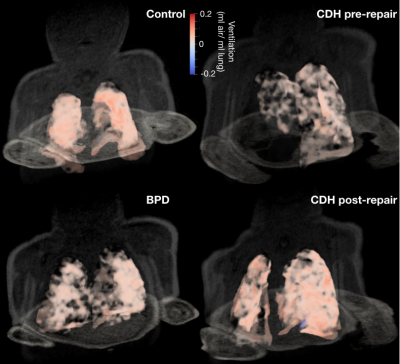 |
Neonatal Lung Ventilation Mapping from Proton Ultrashort Echo-Time MRI
Alister J Bates1, Nara S Higano1, Andreas Schuh2, Andrew Hahn3, Katie J Carey3, Sean B Fain3, Paul Kingma4, and Jason C Woods1
1Center for Pulmonary Imaging, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 2Biomedical Image Analysis Group, Imperial College London, London, United Kingdom, 3Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 4Bronchopulmonary Dysplasia (BPD) Center, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States
Neonatal lung disease is often related to premature birth or congenital abnormalities. Structural MRI has been performed in these patients but does not indicate which lung regions perform gas exchange. Registered respiratory gated ultra-short echo-time proton MRI can produce lung ventilation maps in neonates throughout the respiratory cycle. This technique showed clear differences between a control subject and 2 patients with lung disease in terms of ventilation efficiency (inhaled air per milliliter of lung), spatial and temporal ventilation homogeneity. Further differences were shown post-surgical intervention, demonstrating the method and as a potential means to assess treatment efficacy.
|
0085.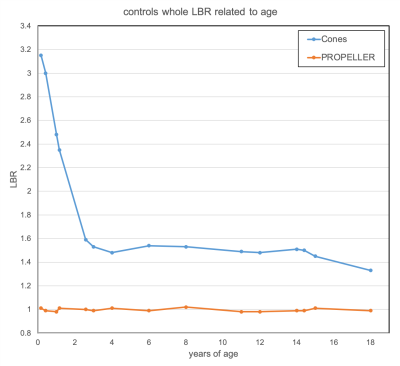 |
3D UTE Cones for assessing lung density in paediatric cases
Konstantinos G. Zeimpekis1, Florian Wiesinger2, Gaspar Delso2, Julia Geiger3, and Christian Kellenberger4
1Nuclear Medicine, University Hospital Zurich, Zurich, Switzerland, 2GE Healthcare, Chicago, IL, United States, 3University Children's Hospital Zurich, Zurich, Switzerland, 4Radiology, University Children's Hospital Zurich, Zurich, Switzerland
3D ultrashort echo-time Cones is tested against PROPELLER for lung density detection in paediatric cases on two cohorts: patients with morphologically normal lungs and patients with Cystic Fibrosis. Cones seems to be able to detect lung density based on lung-to-background signal intensities ratio (LBR) while PROPELLER fails to show any correlation. Cones is able to show the lung anteroposterior gravity gradient as well. There was no difference between Cones LBR of controls and CF while pixel-intensity histogram analysis of Cones slices seem to differentiate pathological from normal lung. Qualitatively, lung constrast decreases with increasing age.
|
|
0086.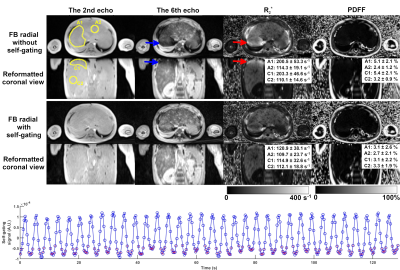 |
Free-Breathing Volumetric Liver R2* Quantification in Pediatric Patients Using 3D Self-Gating Motion-Compensated Stack-of-Radial MRI
Xiaodong Zhong1, Houchun H Hu2, Tess Armstrong3,4, Marcel D Nickel5, Stephan A.R. Kannengiesser5, Vibhas Deshpande6, Berthold Kiefer5, and Holden H Wu3,4
Video Permission Withheld
1MR R&D Collaborations, Siemens Healthcare, Los Angeles, CA, United States, 2Department of Radiology, Nationwide Children's Hospital, Columbus, OH, United States, 3Department of Radiological Sciences, University of California Los Angeles, Los Angeles, CA, United States, 4Department of Physics and Biology in Medicine, University of California Los Angeles, Los Angeles, CA, United States, 5MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany, 6MR R&D Collaborations, Siemens Healthcare, Austin, TX, United States
Liver fat and iron quantification is of growing interest. However, it is challenging and sometimes impossible to perform breath-hold MRI acquisitions in children. Using a breath-hold 3D Cartesian method as reference, a self-gating free-breathing 3D stack-of-radial liver R2* quantification technique was evaluated. Results showed that the free-breathing stack-of-radial technique accurately quantified fat even without self-gating, while free-breathing R2* quantification had biases caused by respiratory motion and self-gating was necessary for accurate R2* quantification in pediatric subjects. This technique has potential for accurate and efficient free-breathing quantification of both liver fat and iron in pediatric patients.
|
|
 |
0087.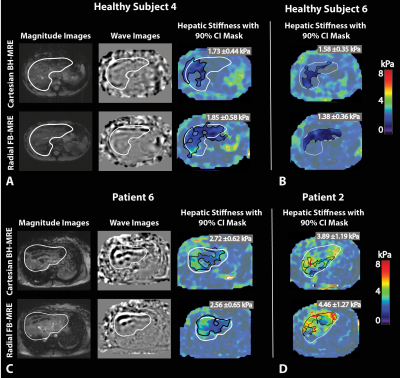 |
Assessment of Free-Breathing Radial Magnetic Resonance Elastography in Healthy Children and Children with Liver Disease at 3T
Sevgi Gokce Kafali1,2, Tess Armstrong1, Shu-Fu Shih1,2, Joseph L Holtrop3, Robert S Venick4, Shahnaz Ghahremani1, Bradley D. Bolster Jr5, Claudia M. Hillenbrand3, Kara L. Calkins4, and Holden H. Wu1,2
1Radiological Sciences, University of California, Los Angeles, Los Angeles, CA, United States, 2Bioengineering, University of California, Los Angeles, Los Angeles, CA, United States, 3Diagnostic Imaging, St. Jude Children’s Research Hospital, Memphis, TN, United States, 4Pediatrics, University of California, Los Angeles, Los Angeles, CA, United States, 5Siemens Medical Solutions, Salt Lake City, UT, United States
Hepatic stiffness measured by magnetic resonance elastography (MRE) is a biomarker that correlates with histopathological staging of liver fibrosis. Conventional Cartesian gradient-echo MRE requires breath-holding (BH), which may be inconsistent and challenging for children. Free-breathing (FB) MRE based on radial acquisition is a promising solution to this problem. In this study, we investigated the agreement in hepatic stiffness values from BH-MRE and FB-MRE, as well as repeatability, in healthy children and pediatric patients at 3T. Bland-Altman analysis showed a high level of agreement between BH-MRE and FB-MRE, and repeatability analysis showed similar performance for BH-MRE and FB-MRE.
|
0088.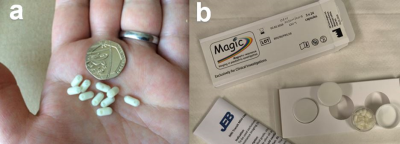 |
A first-in-child feasibility study of a new mini-capsule medical device to measure whole gut transit in pediatric constipation using MRI (MAGIC)
Hayfa Sharif1,2, Nichola Abrehart1, Caroline Hoad1,3, Kathryn Murray1,3, Alan Perkins1,4, Penny Gowland3, Robin Spiller1, Roy Harris1, Sian Kirkham5, Sabarinathan Loganathan5, Michalis Papadopoulos5, Young Persons Advisory Group (YPAG)6, David Devadason5,
and Luca Marciani1
1Nottingham Digestive Diseases Centre and NIHR Nottingham Biomedical Research Centre, University of Nottingham, Nottingham, United Kingdom, 2Clinical Radiology, Amiri Hospital, Ministry Of Health, Civil Service Commission, Kuwait, 3Sir Peter Mansfield Imaging Centre, School of Physics and Astronomy, University of Nottingham, Nottingham, United Kingdom, 4Medical Physics and Clinical Engineering, Nottingham University Hospitals, Queen’s Medical Centre, Nottingham, United Kingdom, 5Nottingham Children’s Hospital, Nottingham University Hospitals NHS Trust, Queen’s Medical Centre, Nottingham, United Kingdom, 6NUH YPAG, Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
We developed a new MRI mini-capsule marker device to measure whole gut transit (WGTT) in pediatric constipation to overcome image quality and ionizing radiation limitations of current X-ray methods. Thirty five healthy children and 16 patients with constipation were asked to swallow a number of mini-capsules and imaged, following a common X-ray radiopaque marker protocol. The capsules were imaged successfully in the colon. WGTT was calculated from the capsules count and was significantly longer in the patients compared to the controls. The study also showed excellent feasibility and safety of using the new device and methods in children with constipation.
|
|
 |
0089.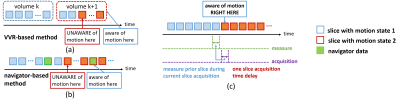 |
Improved data quality and reduced costs by slice localization integrated MRI monitoring
Yao Sui1,2, Onur Afacan1,2, Ali Gholipour1,2, and Simon Keith Warfield1,2
1Harvard Medical School, Boston, MA, United States, 2Boston Children's Hospital, Boston, MA, United States
Motion monitoring has shown helpful in MRI, particularly in long acquisitions such as 2D echo-planar imaging for fMRI. The most widely-used motion monitoring for fMRI relies on volume-to-volume registration (VVR). However, motion happens at the slice level, and VVR is insufficiently sensitive to intra-volume motion. In this work, we present the first slice-by-slice self-navigated motion monitoring system for MRI via a real-time slice-to-volume registration (SVR) algorithm. Extensive experiments demonstrated that our approach provides accurate motion measurements, and allows adaptive acquisition that ensures sufficient amount of data, while not acquiring data in excess, leading to improved data quality and reduced costs.
|
0090.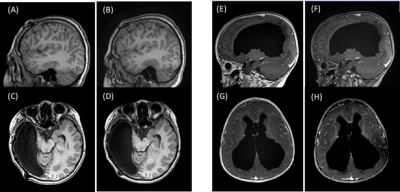 |
Fast scan with a wave-CAIPI MPRAGE sequence to minimize motion artifacts in pediatric T1-weighted imaging
Emi Niisato1, Yung-Chieh Chen2, Shojen Cheng2, Yi-Hsin Wang2, Wei Liu3, Daniel Nicolas Splitthoff4, and Cheng-Yu Chen2
1Siemens Healthcare Limited, Taipei, Taiwan, 2Department of Medical Imaging, Taipei Medical University Hospital, Taipei, Taiwan, 3Siemens Shenzhen Magnetic Resonance Ltd, Shenzhen, China, 4Siemens Healthineers AG, Erlangen, Germany Pediatric magnetic resonance imaging (MRI) needs extra care since patients cannot remain still for long in the MRI bore. Therefore, scans should be performed as quickly as possible. Our study investigated the role of fast T1 3D Magnetization Prepared Rapid Acquisition Gradient Echo (MPRAGE) scans using wave-controlled aliasing with parallel imaging (wave-CAIPI) in pediatric patients. We presented that scan times were shortened significantly, and images had fewer motion artifacts compared with conventional MPRAGE images. We further evaluated contrast-to-noise ratios (CNRs) in five cerebellar areas and saw no significant differences between the conventional and wave-CAIPI MPRAGE images. |

 Back to Program-at-a-Glance
Back to Program-at-a-Glance Watch the Video
Watch the Video Back to Top
Back to Top