Digital Posters
Fat & Metabolism II
ISMRM & SMRT Annual Meeting • 15-20 May 2021

| Concurrent 4 | 15:00 - 16:00 |
3851.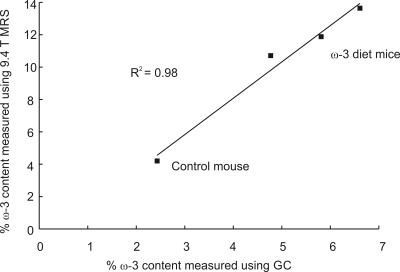 |
Comparing omega-3 content in adipose tissue of mice and rats fed a high omega-3 diet with MRS at 9.4T
Clara J. Fallone1, Anthony G. Tessier1,2, Catherine J. Field3, and Atiyah Yahya1,2
1Department of Oncology, University of Alberta, Edmonton, AB, Canada, 2Department of Medical Physics, Cross Cancer Institute, Edmonton, AB, Canada, 3Department of Agricultural, Food and Nutritional Science, University of Alberta, Edmonton, AB, Canada
Omega-3 (ω-3) fat intake is important to disease and reflected in adipose tissue composition. Optimized PRESS (Point RESolved Spectroscopy) at 9.4T is used to quantify relative ω-3 fat content in adipose tissue of mice and rats fed a 16% ω-3 diet and in a control diet mouse. The actual ω-3 fat content in the mice was determined using gas chromatography and compared to that obtained using optimized MRS (R2 = 0.98). On average, the % ω-3 content measured with MRS in rat adipose tissue was approximately 39% higher than that in mouse.
|
|||
3852.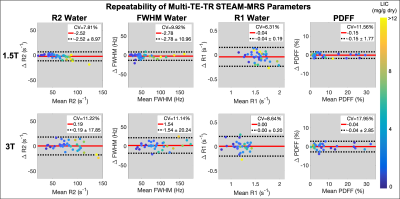 |
Precision of STEAM-MRS for Multi-Parametric Quantification in Subjects with Liver Iron Overload at 1.5T and 3T
Gregory Simchick1,2, Ruiyang Zhao1,2, Gavin Hamilton3, Scott Reeder1,2,4,5,6, and Diego Hernando1,2,4
1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 3Radiology, University of California-San Diego, San Diego, CA, United States, 4Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Medicine, University of Wisconsin-Madison, Madison, WI, United States, 6Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
The precision (repeatability and reproducibility) of quantitative stimulated echo acquisition mode (STEAM) MRS was evaluated in subjects with known or suspected liver iron overload at both 1.5T and 3T. The test-retest repeatability and reproducibility across acquisition modes (multi-TE vs multi-TE-TR) of STEAM-MRS multi-parametric quantification was evaluated using linear regression and Bland-Altman analyses. STEAM-MRS demonstrated high precision for several biomarkers, including R2water and R2fat, FWHMwater and FWHMfat as surrogates for R2*, and PDFF, at both 1.5T and 3T. R1water and R1fat exhibited moderate repeatability. The precision of the water estimates (R1, R2, and FWHM) was
relatively similar at both field strengths.
|
|||
3853.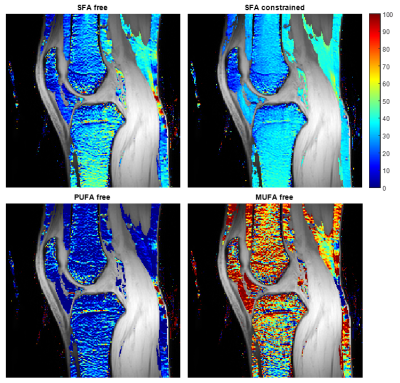 |
Fatty acid composition quantification in bone marrow at 7 T: method comparison and in vivo feasibility
Sevgi Emin1, Jonas Svensson1,2, Martin Englund3, and Pernilla Peterson1,2
1Medical Radiation Physics, Department of Translational Medicine, Lund University, Malmo, Sweden, 2Medical Imaging and Physiology, Skane University Hospital, Lund, Sweden, 3Orthopaedics, Department of Clinical Sciences Lund, Lund University, Lund, Sweden
Chemical shift-encoded magnetic resonance imaging may be used to estimate the fatty acid composition (FAC) of bone marrow adipose tissue (BMAT), and the method may benefit from the improved spectral resolution at ultra-high field strength. In this work, the in vivo feasibility of FAC quantification in BMAT at 7 T was investigated, and simulations were used to determine the optimal image acquisition parameters and reconstruction model. The study showed that using a short inter-echo time, FAC quantification in BMAT was feasible and robust at 7 T, and that the noise performance might be improved using a constrained reconstruction model.
|
|||
3854.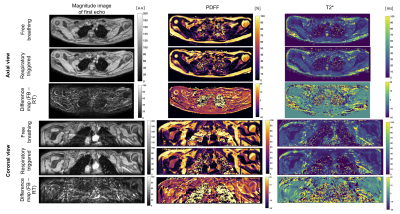 |
Breathing-induced B0 fluctuations bias proton density fat fraction and T2* mapping of brown adipose tissue in the supraclavicular fossa
Mingming Wu1, Cora Held1, Maximilian N. Diefenbach1,2, Jakob Meineke3, Aashley S.D. Sardjoe Mishre4,5, Kilian Weiss6, Hermien E. Kan5, Daniela Junker1, Hans Hauner7,8, and Dimitrios C. Karampinos1
1Department of Diagnostic and Interventional Radiology, School of Medicine, Technical University of Munich, Munich, Germany, 2Division of Infectious Diseases and Tropical Medicine, University Hospital, LMU Munich, Munich, Germany, 3Philips Research Lab, Hamburg, Germany, 4Division of Endocrinology and Einthoven Laboratory for Experimental Vascular Medicine, Department of Medicine, Leiden University Medical Center, Leiden, Netherlands, 5Department of Radiology, C.J. Gorter Center for High Field MRI, Leiden University Medical Center, Leiden, Netherlands, 6Philips Healthcare, Hamburg, Germany, 7Else Kröner Fresenius Center for Nutritional Medicine, School of Life Sciences, Technical University of Munich, Munich, Germany, 8Institute for Nutritional Medicine, School of Medicine, Technical University of Munich, Munich, Germany
Proton density fat fraction and T2* mapping have been used to characterize fat tissue in the human supraclavicular fossa with the aim of detecting brown adipose tissue and its response to activation by changes of the two. However, chemical shift encoding-based water-fat separation in that region has been primarily performed in free-breathing mode. The present work reports on breathing-induced B0 fluctuations in the human supraclavicular fossa, and the severe bias introduced on both PDFF and T2* quantification, as shown with simulated B0 fluctuation effects. The effect of respiratory triggering on artefact reduction is investigated in a cohort of 13 volunteers.
|
|||
3855.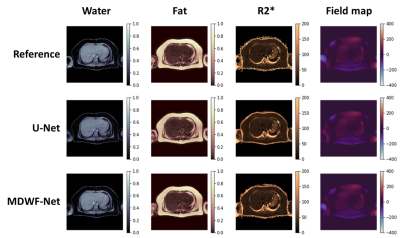 |
Water/fat separation using multiple decoder U-Net architecture (MDWF-Net) for accurate R2* measurements
Juan Pablo Meneses1,2, Cristobal Arrieta1,2, Gabriel della Maggiora1,2, Pablo Irarrazaval1,2,3,4, Cristian Tejos1,2,4, Marcelo Andia1,2,5, Carlos Sing Long1,2,3,6,7, and Sergio Uribe1,2,5
1Biomedical Imaging Center, Pontificia Universidad Catolica de Chile, Santiago, Chile, 2ANID – Millennium Science Initiative Program – Millennium Nucleus for Cardiovascular Magnetic Resonance, Santiago, Chile, 3Institute for Biological and Medical Engineering, Pontificia Universidad Catolica de Chile, Santiago, Chile, 4Department of Electrical Engineering, Pontificia Universidad Catolica de Chile, Santiago, Chile, 5Radiology Department, School of Medicine, Pontificia Universidad Catolica de Chile, Santiago, Chile, 6Institute for Mathematical & Computational Engineering, Pontificia Universidad Catolica de Chile, Santiago, Chile, 7ANID – Millennium Science Initiative Program – Millennium Nucleus for Discovery of Structure in Complex Data, Santiago, Chile
Proton density fat fraction (PDFF) and $$$R_2^*$$$, key biomarkers associated to liver disease, can be obtained by solving the water/fat separation problem. Convolutional Neural Networks (CNN) have been proposed for solving this problem. However, proposed solutions have not achieved accurate $$$R_2^*$$$ mapping. We introduce MDWF-Net, a CNN model for computing high quality water-fat, $$$R_2^*$$$ and field mapping from abdominal acquisitions. The results were evaluated considering error and structural similarity and compared against a U-Net. We also evaluated ROIs in the liver for PDFF and $$$R_2^*$$$. The proposed MDWF-Net overperforms the original U-Net, especially for $$$R_2^*$$$ maps, even with fewer echoes.
|
|||
3856.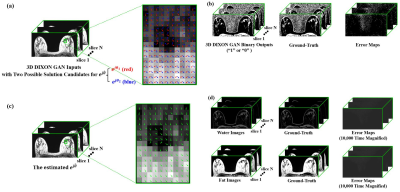 |
The video domain transfer deep learning network with error correction for Dixon Imaging with consistent slice-to-slice water and fat separation
Jong Bum Son1, David Rauch1, Bikash Panthi1, Zijian Zhou1, Benjamin Musall1, Marion Scoggins2, Mark Pagel3, and Jingfei Ma1
1Imaging Physics Department, The University of Texas MD Anderson Cancer Center, Houston, TX, United States, 2Diagnostic Radiology Department, The University of Texas MD Anderson Cancer Center, Houston, TX, United States, 3Cancer Systems Imaging Department, The University of Texas MD Anderson Cancer Center, Houston, TX, United States
We applied a video processing deep-learning neural network (originally developed to synthesize high resolution photorealistic video from a time series of dancing poses, semantically segmented street-view labels, or human face outline sketches) to Dixon imaging to present combined benefits of 2D and 3D networks. The developed Dixon Video Domain Transfer Generative Adversarial Network (DixonVDTGAN) could create slice-to-slice consistent water images with reduced demand on GPU memory. It could also successfully correct deep-learning processing errors for robust water and fat signal separation under two assumptions that the deep-learning processing errors are localized and the image phase is spatially smooth.
|
|||
3857.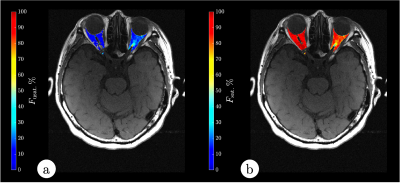 |
Orbit Fat Quant with PASTA and Unsaturated- and Saturated-Fat Opposed Phase.
Vadim Malis1, Asako Yamamoto1, Yoshimori Kassai2, Won Bae1, Marianne McDonald3, and Mitsue Miyazaki1
1Radiology, UC San Diego, San Diego, CA, United States, 2Canon Medical, Tochigi, Japan, 3UC San Diego, San Diego, CA, United States
In general, orbit fat suppression is not achieved due to the presence of unsaturated fat signals near water resonance. We have developed PASTA with unsaturated and saturated fat opposed phase (USOP) like a Dixon method. Semi-quantitative analysis shows about 6 – 18% of unsaturated fat in the orbits. Interestingly, two subjects having lazy eye (amblyopia) with double visions (diplopia) shows decreased in unsaturated fat signal.
|
|||
3858.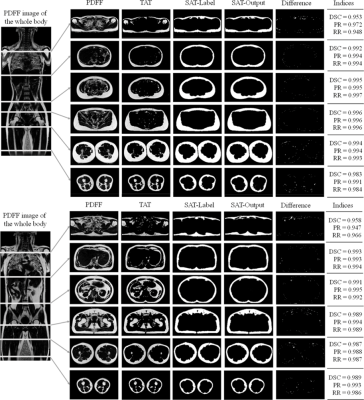 |
Segmentation of whole-body adipose tissue from magnetic resonance fat-fraction images with U-net deep-learning framework
Chuanli Cheng1, Zhiming Wang1, Qian Wan1, Yangzi Qiao1, Changjun Tie1, Hairong Zheng1, Xin Liu1, and Chao Zou1
1Shenzhen Institutes of Advanced Technology,Chinese Academy of Sciences, Shenzhen, China
Over the past several decades, the worldwide obesity epidemic has become a significant public health. As a consequence, accurate measurement of obesity is critical for obesity management. In the present study, an automated algorithm is proposed to segment subcutaneous adipose tissue (SAT) and internal adipose tissue (IAT) from the total adipose tissue for whole-body fat distribution analysis using proton density fat fraction (PDFF) magnetic resonance images. The dice coefficient of the network achieved 97.6%, and the processing time was less than 0.1s/image.
|
|||
3859.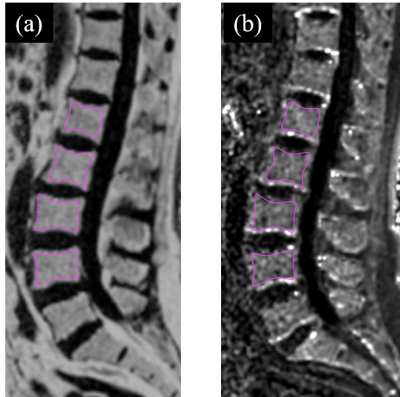 |
3D FACT Sequence Based Proton Density Fat Fraction Combined with Marrow R2* for Osteopenia and Osteoporosis Assessment
Guanwu Li1, Wenshen Zhou2, Shixin Chang1, Dongmei Wu3, and Yongming Dai2
1Department of Radiology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China, 2Central Research Institute, United Imaging Healthcare, Shanghai, China, 3Shanghai Key Laboratory of Magnetic Resonance, School of Physics and Electronics Science, East China Normal University, Shanghai, China
Marrow proton density fat fraction (PDFF) and R2* at the lumbar spine in postmenopausal females of widely varying bone density were simultaneously measured with a 3D Fat Analysis & Calculation Technique (FACT) Sequence at 3.0T. Discrimination of osteopenia and osteoporosis can be improved with a combination of the PDFF and R2*.
|
|||
3860.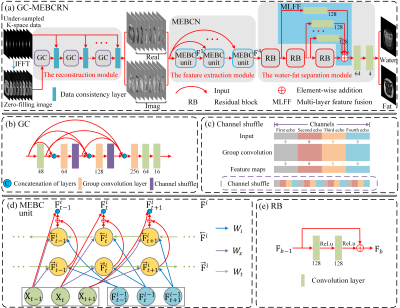 |
Accelerated water-fat separation based on deep learning model exploring multi-echo nature of mGRE
Qinjia Bao1, Xiaojun Li2, Kewen Liu2, Zhao Li3, Hongxia Xiong2, Jingjie Yan4, Yalei Chen2, and Chaoyang Liu3
1Weizmann Institute of Science, Rehovot, Israel, 2School of Information Engineering, Wuhan University of Technology, Wuhan, China, 3State Key Laboratory of Magnetic Resonance and Atomic and Molecular Physics, Wuhan Center for Magnetic Resonance, Wuhan Institute of Physics and Mathematics, Innovation Academy for Precision Measurement Science and Technology, Wuhan, China, 4Huazhong University of Science and Technology, Wuhan, China
We proposed a novel deep learning network for water-fat separation from undersampled mGRE data. The network contains three components: The first is the reconstruction module, which can effectively take advantage of the similarity between different echoes to recover the fully sampled image from the undersampled data; the second is the feature extraction module, which learns the correlations between consecutive echoes; and the third is the water-fat separation module that processes the feature information extracted from the feature extraction module. The results show that the proposed network can effectively obtain high-quality water and fat images at 6 times acceleration.
|
|||
3861.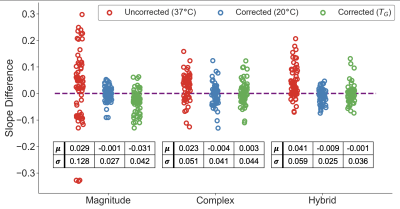 |
Temperature-Corrected Proton Density Fat Fraction Estimation using Magnitude, Complex, and Hybrid Chemical Shift-Encoded MRI in Phantoms
Ruvini Navaratna1,2, Ruiyang Zhao1,2, Timothy J Colgan2, Houchun Harry Hu3, Mark Bydder4, Takeshi Yokoo5, Mustafa R Bashir6,7,8, Michael S Middleton9, Suraj D Serai10, Dariya Malyarenko11, Thomas Chenevert11, Mark Smith3, Walter Henderson9,
Gavin Hamilton9, Yunhong Shu12, Claude B Sirlin9, Jean Tkach13, Andrew T Trout13,14, Jean H Brittain15, Diego Hernando1,2, and Scott B Reeder1,2,16,17,18
1Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Radiology, University of Wisconsin - Madison, Madison, WI, United States, 3Radiology, Nationwide Children's Hospital, Columbus, OH, United States, 4Radiological Sciences, University of California - Los Angeles, Los Angeles, CA, United States, 5Radiology, University of Texas - Southwestern Medical Center, Dallas, TX, United States, 6Radiology, Duke University Medical Center, Durham, NC, United States, 7Division of Hepatology, Duke University Medical Center, Durham, NC, United States, 8Center for Advanced Magnetic Resonance Development, Duke University Medical Center, Durham, NC, United States, 9Radiology, University of California - San Diego, San Diego, CA, United States, 10Radiology, Children's Hospital of Philadelphia, Philadelphia, PA, United States, 11Radiology, University of Michigan, Ann Arbor, MI, United States, 12Radiology, Mayo Clinic, Rochester, MN, United States, 13Radiology, Cincinnati Children's Hospital and Medical Center, Cincinnati, OH, United States, 14Radiology, University of Cincinnati College of Medicine, Cincinnati, OH, United States, 15Calimetrix, LLC, Madison, WI, United States, 16Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States, 17Medicine, University of Wisconsin - Madison, Madison, WI, United States, 18Emergency Medicine, University of Wisconsin - Madison, Madison, WI, United States
Chemical shift-encoded (CSE) MRI is a well-established technique to quantify proton density fat-fraction (PDFF) as a quantitative imaging biomarker of hepatic steatosis. However, temperature is known to affect the accuracy and precision of PDFF quantification in phantoms. Previous work has demonstrated the benefit of temperature-correction using magnitude-based CSE-MRI PDFF estimation. However, the effect of temperature correction on complex- and hybrid-based CSE-MRI PDFF estimation is unknown. In this study, we aim to compare the effects of PDFF temperature-correction for magnitude-based, complex-based, and hybrid-based CSE-MRI using simulations, temperature-controlled phantom experiments, and a multi-center phantom study.
|
|||
3862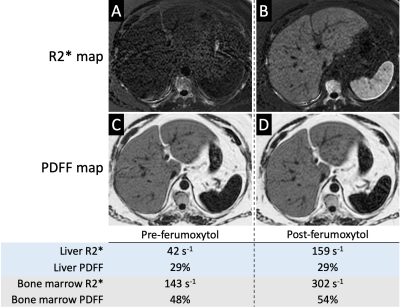 |
Linearity and Bias of Liver and Bone Marrow Proton Density Fat Fraction (PDFF) in the setting of Ferumoxytol MRI Video Permission Withheld
Ali Pirasteh1, Srijyotsna Volety1, Matthias R Muhler2, Diego Hernando1, and Scott B Reeder3
1Radiology and Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3Radiology, Medical Physics, Biomedical Engineering, Medicine, Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
We evaluated the robustness of measuring liver and bone marrow PDFF by chemical shift encoded (CSE) MRI measured before and 1-3 days after intravenous (IV) administration of ultra-small superparamagnetic iron oxide (USPIO) particles, i.e., ferumoxytol, as IV contrast. Among the eight included subjects, there was strong linearity and no significant bias between pre- and post-ferumoxytol CSE-MRI liver PDFF (R2=0.99, slope=0.99 and intercept=0.38%; mean bias [limits of agreement]=0.4% [±1.7] at 1.5T, and 0.2% [±1.7] at 3.0T. However, CSE-MRI bone marrow PDFF suffered from bias and overestimation post-ferumoxytol (R2=0.85, slope=0.85, intercept=12.8%, mean bias [LOA]=5.4% [±6.2] at 1.5T and 4.4% [±6.5] at 3.0T).
|
|||
3863.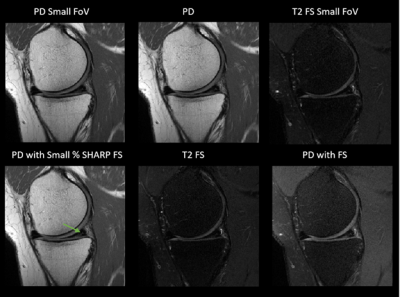 |
Spectral-Heterogeneity-Adaptive Radiofrequency Pulses for Improving the Conspicuity of Meniscal Tears at 3T and 7T
Venkata Veerendranadh Chebrolu1, Peter Kollasch1, Daniel B Spence2, Joel P Felmlee2, Benjamin M Howe2, Matthew A Frick2, and Kimberly K Amrami2
1Siemens Medical Solutions USA, Inc., Rochester, MN, United States, 2Department of Radiology, Mayo Clinic, Rochester, MN, United States
In this work, we evaluate the efficacy of Spectral-Heterogeneity-Adaptive Radiofrequency Pulses (SHARP)-based partial fat saturation for improving meniscal pathology conspicuity at 3T and 7T. Under the guidelines of an IRB, 11 subjects with knee meniscal pathology detected on a previous 3T MRI were imaged at 3T and 7T using six different turbo spin-echo–based MRI imaging options that included SHARP. Two fellowship-trained musculoskeletal radiologists evaluated meniscal pathology conspicuity and selected the top three preferred options for each case. SHARP improved conspicuity of meniscal pathology at 3T and 7T and was within top three preferred options for the highest number of times.
|
|||
3864.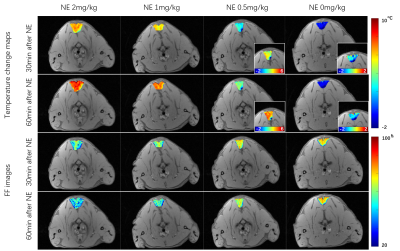 |
Magnetic resonance thermometry in activated interscapular brown adipose tissue of rats with various dose of norepinephrine
Chuanli Cheng1, Qian Wan1, Yangzi Qiao1, Changjun Tie1, Xin Liu1, Hairong Zheng1, and Chao Zou1
1Shenzhen Institutes of Advanced Technology,Chinese Academy of Sciences, Shenzhen, China
Magnetic Resonance thermometry (MRT) in activated brown adipose tissue (BAT) is able to measure the BAT function directly. A previous proposed fat-referenced 1H proton resonance frequency shift MRT method is adopted to compare the thermogenic capacity of rats injected with different dose of norepinephrine (NE). It is found that the rats with 2mg/kg and 1mg/kg NE injection had comparable maximum temperature rises after NE injection (7.1oC vs. 6.7oC), while temperature rises for rats with NE of 0.5mg/kg was significantly lower (3.8oC).
|
|||
3865.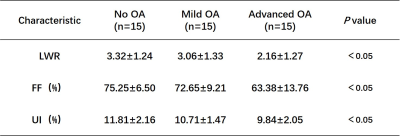 |
Quantitative evaluation of infrapatellar fat pad in knee osteoarthritis by using hydrogen proton MR spectroscopy (1H-MRS)
Lijie Zhong1, Mainwen Li1, Yukun Ding1, Xintao Zhang1, Yanjun Chen1, Yingjie Mei2, and Xiaodong Zhang1
1Department of Medical Imaging, The Third Affiliated Hospital of Southern Medical University, Guangzhou, China, 2China International Center, Philips Healthcare, Guangzhou, China
Infrapatellar fat pad (IPFP) is an adipose structure of knee joint, which plays an important role in the progression of knee osteoarthritis(KOA). In this paper, we evaluate the fat content and composition of the IPFP in normal subjects and different stages of knee osteoarthritis patients using hydrogen proton MR spectroscopy (1H-MRS). In addition, we investigate the relationship between the fat content and composition of the IPFP and Hoffa-synovitis. The results showed that the quantitative parameters of the IPFP by MRS were correlated with the progression of KOA and Hoffa-synovitis.
|
|||
3866.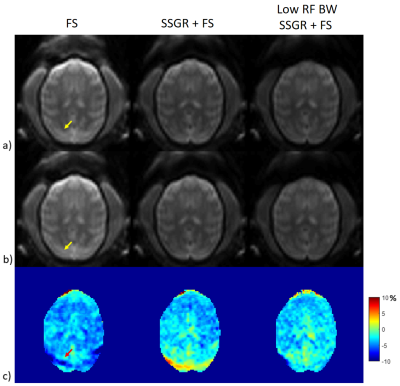 |
Robust Fat Suppression with Slice Selective Gradient Reversal (SSGR) in Amide Proton Transfer Imaging – Application to Non-Human Primate Brain
Hahnsung Kim1,2, Lisa C. Krishnamurthy 3,4, Jinsuh Kim5, and Phillip Zhe Sun1,2
1Yerkes Imaging Center, Yerkes National Primate Research Center, Emory University, Atlanta, GA, United States, 2Department of Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, GA, United States, 3Center for Visual and Neurocognitive Rehabilitation, Atlanta VA, Decatur, GA, United States, 4Department of Physics & Astronomy, Georgia State University, Atlanta, GA, United States, 5Department of Radiology, University of Alabama Birmingham, Birmingham, AL, United States
Single-shot EPI imaging has become a widely used acquisition method in amide proton transfer (APT) imaging due to its fast imaging readout. Because APT effects are relatively small, fat artifacts may significantly impact the asymmetry analysis. Recently, a slice selective gradient reversal (SSGR) method has been reported to effectively suppress fat signals. This work aims to introduce the SSGR method into spin-echo EPI APT imaging, which can be used for fat suppression in the non-human primate brain with substantial pericranial fat.
|
|||
3867.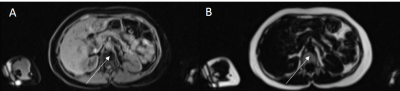 |
Bone Marrow Adiposity Evaluation using Dixon MRI Fat Fraction with Machine Leaning Segmentation in the UK Biobank – Initial Validation
David M Morris1, Chengjia Wang1, Giorgos Papanastasiou2, Calum Gray3, Scott IK Semple1, Tom MacGillivray1, and William Cawthorn1
1Centre for Cardiovascular Science, University of Edinburgh, Edinburgh, United Kingdom, 2University of Essex, Colchester, United Kingdom, 3Edinburgh Imaging, University of Edinburgh, Edinburgh, United Kingdom
The UK Biobank is a research tissue data bank that contains genetic, health and MRI data. This includes 2-point Dixon sequences allowing for the assessment of fat fraction to evaluate bone marrow adiposity. Bone marrow adipose tissue is a potential biomarker of diseases including osteoporosis and endocrine disorders. Manual processing of this big data is not feasible and automated processes must be developed and validated. Machine Learning has been developed for the automated segmentation of anatomically appropriate bone marrow regions of interest and the extracted Fat Fraction values validated against expected values across different subject groups.
|
|||
3868.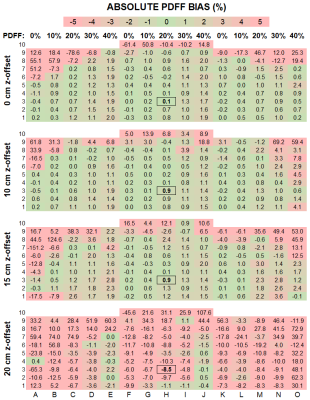 |
Spatial Dependence of PDFF Measurement Bias using Chemical Shift Encoded MRI
Nikolaos Panagiotopoulos1, Thekla Helene Oechtering1, David Rutkowski2, Jean Brittain2, Diego Hernando1,3, and Scott B Reeder1,3,4
1Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Calimetrix LLC, Madison, WI, United States, 3Department of Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 4Departments of Biomedical Engineering, Medicine, and Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
A phantom placed alongside a patient, i.e., “pocket phantom,” can enable quality assurance of proton density fat fraction (PDFF) measurements. To determine the optimal positioning, the spatial dependence of PDFF measurements must be understood. To address this unmet need, we filled the bore of a 3T MRI with pocket phantoms. Though PDFF bias was low, it increased with distance from isocenter. Absolute bias was <2.5% within 18cm (in-plane) and within 10cm (z-direction). We conclude that the optimal position for a PDFF pocket phantom is on the table, centered below the patient at the level of the examined organ.
|
|||
3869.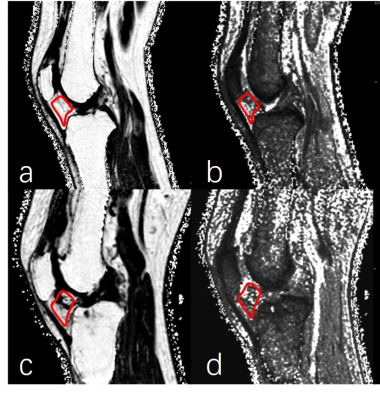 |
Fat fraction and T2* evaluation of the Infrapatellar Fat Pad in Varying Degrees of Knee Osteoarthritis
Yanjun Chen1, Xintao Zhang1, Mianwen Li1, Lijie Zhong1, Jian Wang1, Yingjie Mei2, and Xiaodong Zhang1
1The Third Affiliated Hospital, Southern Medical University, Guangzhou, China, 2China International Center, Philips Healthcare, Guangzhou, China
Knee osteoarthritis (KOA) is characterized by pain and limitation in the range of knee joint motion with resultant disability in a substantial proportion of elderly subjects, and infrapatellar fat pad (IPFP) alterations play an important role in the progress of KOA(1,2). IPFP damage causes a direct change in the proportion of fat in the tissue to water and could be evaluated by magnetic resonance imaging (MRI)(3,4). Fat fraction (FF) and the T2* relaxation time can detect the water and fat changes in IPFP. In this study, IPFP was quantitatively estimated by FF and T2* using modified DIXON (mDIXON) technique.
|
|||
 |
3870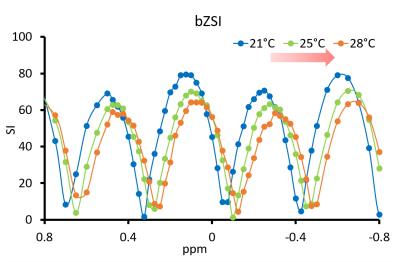 |
A novel method for temperature mapping in fatty tissues based on Z-Spectrum MRI with binomial pulse Video Permission Withheld
Alessandro Scotti1,2, Jin Gao3, Weiguo Li3, Mehran Shaghaghi1, Fred Damen1, and Kejia Cai1,2
1Radiology, University of Illinois at Chicago, Chicago, IL, United States, 2Bioengineering, University of Illinois at Chicago, Chicago, IL, United States, 3Research Resource Center, University of Illinois at Chicago, Chicago, IL, United States
The measurement of temperature in fatty tissues remains a challenge, since the presence of fat protons modifies the phase difference and therefore introduces errors in the quantification from proton resonance frequency shift. By using Z-spectrum MRI, combined with a Jump-Return binomial pulse preparation, we create a sinusoidal variation of the signal as a function of the resonance frequency. The magnitude-based readout eliminates the risk of phase-related artifacts and allows to measure the subtle shifts of water resonance and therefore the temperature, even in fatty tissues. We tested the sequence in mice and cream phantom.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.