Digital Posters
Role of Advanced Imaging in COVID-19
ISMRM & SMRT Annual Meeting • 15-20 May 2021

| Concurrent 6 | 19:00 - 20:00 |
 |
1730.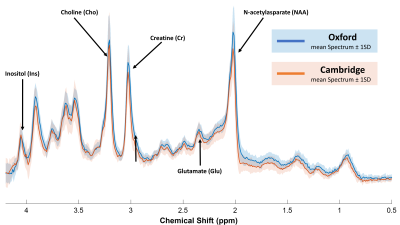 |
Two-site 7T 1H-MRS study in brainstem of “long COVID” patients
Carina Graf1, William T Clarke2, Catarina Rua1, Virginia FJ Newcombe1,3, Victoria C Lupson1, Anne Manktelow3, Doris A Chatfield1, Stephen J Sawcer4, Joanne G Outtrim3, Karen Ersche5, Edward T Bullmore5, David K Menon3, Sarah L Finnegan6,
Rory McDonald6, Stuart Clare6, Martyn Ezra6, Christopher T Rodgers1, Kyle Pattinson6, and James B Rowe4,5,7,8,9
1Wolfson Brain Imaging Centre, Department of Clinical Neurosciences, University of Cambridge, Cambridge, United Kingdom, 2Wellcome Centre for Integrative Neuroimaging, FMRIB, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom, 3Divison of Anaesthesia, Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 4Neurology Unit, Department of Clinical Neurosciences, University of Cambridge, Cambridge, United Kingdom, 5Behavioural and Clinical Neuroscience Institute, Department of Psychiatry, University of Cambridge, Cambridge, United Kingdom, 6Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom, 7Cambridge Centre for Frontotemporal Dementia, Department of Clinical Neurosciences, University of Cambridge, Cambridge, United Kingdom, 8MRC Cognition and Brain Sciences Unit, University of Cambridge, Cambridge, United Kingdom, 9on behalf of the Cambridge NeuroCOVID group and the CITIID-NIHR COVID-19 BioResource Collaboration (www.wbic.cam.ac.uk/neuro-covid/), Cambridge, United Kingdom
SARS-CoV-2 attacks the central nervous system. A particularly nasty symptom of COVID-19 is a feeling of breathlessness that can persist for months after acute infection has subsided (“long COVID”). Based on early MRI observations in hospitalised patients, we hypothesised that COVID-19 may cause inflammation or degeneration of the brainstem where the respiratory control centres are located, leading to these symptoms. In this study we develop a protocol for 1H-MRS in the brainstem on two models of ultra-high field 7T MRI scanner. We show feasibility to profile brainstem neurochemistry in anticipation of a multi-site clinical study across the UK’s 7T centres.
|
||
1731.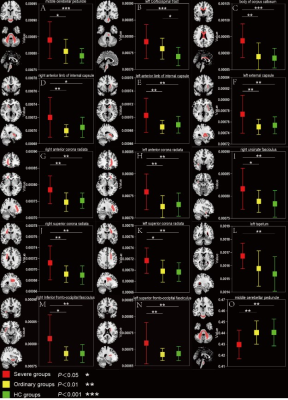 |
A preliminary study of Diffusion tensor imaging in recovered COVID-19 patients
Niu Shanshan1, Xie Qing1, Liao Jianwei1, Li Yingqin1, Qian Long2, Zhang Yaqin1, and Li Shaolin1
1Department of Radiology, the Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai,Guangdong, China, 2MR Research, GE Healthcare, Beijing, China
SARS‐CoV2 has been shown to cause central nervous system (CNS) damages. However, there have been few studies on neurological changes in recovered COVID-19 patients. In current study, we used DTI to assess the potential delayed damages in the CNS of the recovered COVID-19 patients caused by SARS-CoV2. Our results suggested that the microstructural integrity of white matter fibers is disrupted in recovered COVID-19 patients, which provided the evidence of CNS damages.
|
|||
1732.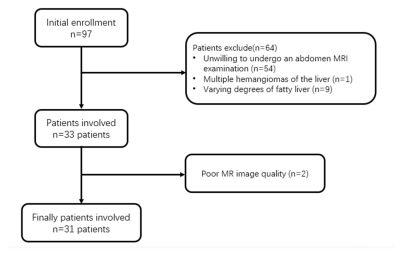 |
Quantitative characterization of liver tissue in COVID-19 recovered patients using T1 mapping, R2* mapping and MRI-PDFF
Wenjun Yu1, Yijie Fang1, Qikun Guo2, Xiaojun Chen3, Wenhao Wu1, Long Qian4, Taoyu Jia5, Kunwei Li1, Chuan Huang6, Bing Wu4, and Shaolin Li1
1Radiology, The Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, China, 2The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China, 3Radiology, The First Affiliated Hospital of Sun Yat-sen University, Zhuhai, China, 4MR Research, GE Healthcare, Beijing, Beijing, China, 5The Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, China, 6Radiology, Stony Brook Medicine, Stony Brook, New York, NY, United States
Liver injuries have been reported with strong evidence in COVID-19 patients. Whether these disturbances are presented in patients recovered from COVID-19 is still unknown. Totally 31 COVID-19 recovered patients were collected. And 37 sex- and age-matched normal controls (NC) were were further recruited. MR imaging was performed using a 3.0T scanner with T1mapping, R2* mapping and proton density fat fraction (PDFF) for all the patients. Abnormal liver T1 and PDFF values, which may be associated with subclinical renal injury due to COVID-19.
|
|||
1733.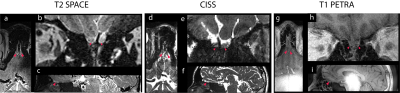 |
Comparing Methods for Ultra-High Resolution Structural Imaging of Human Olfactory Bulb and Tract at 3T
Sichen Ludwig Zhao1,2, Jay A Gottfried2, John A Detre2, and M Dylan Tisdall3
1Bioengineering, School of Engineering and Applied Science, University of Pennsylvania, Philadelphia, PA, United States, 2Neurology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, 3Radiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States
The olfactory bulbs (OBs) and tracts transmit odor information from the nose to the brain and plays a key role in learning, memory, and emotion. In vivo imaging of the human olfactory bulbs (OBs) is inherently challenging due to their limited size and high susceptibility gradients at the basal frontal lobes. We compare three sequences (T2 SPACE, CISS, and T1-weighted PETRA) to produce the highest-resolution (440um) structural images of the human olfactory bulb at 3 T. We demonstrate that these images offer robust visualization of the olfactory bulbs and tracts that projects to the medial temporal lobes.
|
|||
1734.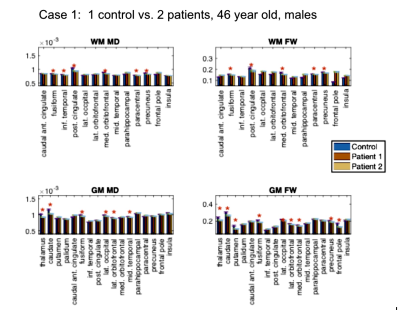 |
COVID19 effects on brain tissue microstructure: Longitudinal study of self-isolated cases using diffusion MRI
J. Jean Chen1,2, Jordan A. Chad1,2, Xiang Ji3, Bradley J. Macintosh1,3, Asaf Gilboa2,4, Eugenie Roudaia2, Allison Sekuler2,4, Benjamin Lam3, Chris Heyn3, Sandra E. Black3, and Simon J. Graham1,3
1Department of Medical Biophysics, University of Toronto, Toronto, ON, Canada, 2Rotman Research Institute, Baycrest Health Sciences, Toronto, ON, Canada, 3Hurvitz Brain Sciences, Sunnybrook Research Institute, Toronto, ON, Canada, 4Department of Psychology, University of Toronto, Toronto, ON, Canada
The impact of COVID19 on the brain’s microstructural integrity is still unclear. In this study, we study self-isolated COVID19 patients using diffusion-tensor and free-water imaging, based on single- and multi-shell acquisitions, respectively. We demonstrate reduced mean diffusivity and free water in both grey and white matter of patients in regions associated with vision and olfaction. At 3-month follow-up, microstructural abnormalities in patients appear to persist, and involve more brain regions, including parts of the default-mode network. Our results support the existence of measurable long-term, evolving brain deficits due to COVID19.
|
|||
1735.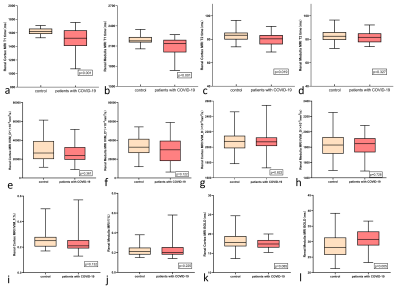 |
Quantitative assessment demonstrates renal changes in COVID-19 recovered patients
Yijie Fang1, Wenjun Yu1, Long Qian2, Chuan Huang3, and Shaolin Li1
1The Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, China, 2MR Research, GE Healthcare, Beijing, China, 3Stony Brook Medicine, Stony Brook, New York, NY, United States
Renal injury has been commonly observed in patients with COVID-19. The effect of the virus on kidneys in COVID-19 recovered patients remains unclear. Thirty-seven COVID-19 recovered patients were Prospectively collected. And 37 sex- and age-matched normal controls (NC) were enrolled. T1 mapping, T2 mapping, BOLD and IVIM for each participant were acquired using 3.0T MRI. The COVID-19 recovered patients demonstrated abnormal renal T1 and T2 and R2* values, which may be associated with subclinical renal injury due to COVID-19.
|
|||
1736.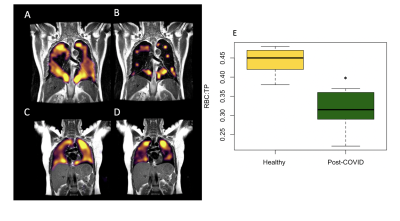 |
Utilizing hyperpolarised xenon MRI to detect gas transport deficiencies in post-COVID lungs
James T. Grist1,2,3, Mitch Chen3, Guilhem J. Collier4, Emily Fraser5, Ling-Pei Ho5,6, and Jim M. Wild4
1Physiology, Anatomy, and Genetics, University of Oxford, Oxford, United Kingdom, 2Centre for Magnetic Resonance, University of Oxford, Oxford, United Kingdom, 3Radiology, Oxford NHS Foundation Trust, Oxford, United Kingdom, 4POLARIS, University of Sheffield, Sheffield, United Kingdom, 5Oxford Interstitial Lung Disease Service, Oxford NHS Foundation Trust, Oxford, United Kingdom, 6MRC Human Immunology Unit, University of Oxford, Oxford, United Kingdom
Test
|
|||
1737.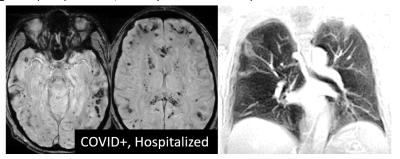 |
NEUROCOVID19: Impact of the Virus on the Brain
Simon J Graham1, J Jean Chen2, Asaf Gilboa2, Brad J Macintosh3, Allison B Sekuler2, Sandra E Black3, Jordan A Chad2, Ivy Cheng4, Rob Fowler4, Fuqiang Gao3, Maged Goubran3, Chinthaka (Chris) Heyn1, Aravinthan (Arv) Jegatheesan1,
Xiang (Patrick) Ji3, Ben Lam3, Mario Masellis3, Jennifer S Rabin3, and Eugenie Roudaia2
1Physical Sciences Platform, Sunnybrook Research Institute, Toronto, ON, Canada, 2Rotman Research Institute, Baycrest, Toronto, ON, Canada, 3Hurvitz Brain Sciences Program, Sunnybrook Research Institute, Toronto, ON, Canada, 4Evaluative Clinical Sciences Platform, Sunnybrook Research Institute, Toronto, ON, Canada
NEUROCOVID19 is a longitudinal observational study to characterize the impact of the SARS-COV-2 virus on brain anatomy and function in individuals who are no longer infectious, using an extensive MRI protocol. Novel aspects include imaging of COVID-19 survivors who either self-isolated or were hospitalized, and control individuals who had cold or flu-like symptoms but tested negative for the virus. Breath-hold ultra-short TE imaging of the lung is also included to study brain-lung relationships. This report describes the study design and initial anatomical findings of the recruited participants (3 hospitalized and 23 self-isolated COVID-19 participants, 11 controls at abstract submission).
|
|||
1738.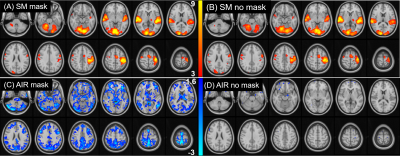 |
Effect of Wearing a Face Mask on fMRI BOLD Contrast
Christine S W Law1, Patricia S Lan2, and Gary H Glover2
1Stanford University, Palo Alto, CA, United States, 2Stanford University, Stanford, CA, United States
The widespread incidence of infection from the novel coronavirus SARS-CoV-2 has prompted many research MRI facilities to require scan subjects to wear masks during scanning in order to diminish the risk of virus transmission. Wearing an efficacious mask will mix some expired air with fresh air, and lead to increased carbon dioxide concentration [CO2] in inspired air. The question we approached is: Since CO2 is a potent vasodilator, does this elevation in [CO2] alter functional MRI (fMRI)?
|
|||
1739. |
Feasibility of Single Breath-hold Isotropic Voxel 129Xe MRI in COVID-19 Survivors using a Key-Hole Method.
Tuneesh K. Ranota1, Hacene Serrai2, David G. McCormack3, Grace Parraga1,4,5, and Alexei Ouriadov1,2,6
1School of Biomedical Engineering, Faculty of Engineering, The University of Western Ontario, London, ON, Canada, 2Department of Physics and Astronomy, The University of Western Ontario, London, ON, Canada, 3Division of Respirology, Department of Medicine, The University of Western Ontario, London, ON, Canada, 4Robarts Research Institute, London, ON, Canada, 5Department of Medical Biophysics, The University of Western Ontario, London, ON, Canada, 6Lawson Health Research Institute, London, ON, Canada
Hyperpolarized 129Xe gas lung MRI is an efficient technique used to investigate and assess pulmonary diseases. To improve the performance of 129Xe MRI in lung imaging a method for high-resolution 3D static ventilation images using FGRE combined with the key-hole method in a single breath-hold, was proposed. This technique acquires high-resolution 129Xe 3D static ventilation isotropic-voxel images from the COVID-19 survivors in a single breath-hold. The SNR of the images allowed for the analysis of VDP. This study confirms the feasibility of using isotropic-voxel acquisition sequence in a single breath-hold MRI to study the effects of COVID-19 on the lungs.
|
|||
1740.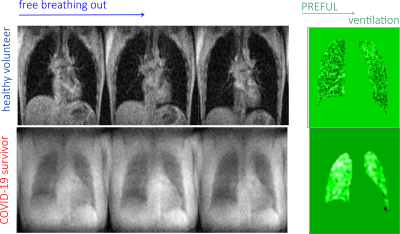 |
Proof-of-principal of 1H PREFUL approaches at 0.5T: lung ventilation and perfusion maps of a healthy volunteer and a Covid-19 survivor
Arthur Harrison1, Galina E Pavlovskaya1,2, Thomas Meersmann1, Olga S Pavlova3,4, Alexander Makurenkov4, Yury A Pirogov4, and Nikolay V Anisimov3,4
1SPMIC/Medicine, University of Nottingham, Nottingham, United Kingdom, 22Nottingham NIHR Biomedical Research Centre, Nottingham, United Kingdom, 3Faculty of Fundamental Medicine, Lomonosov Moscow State University, Moscow, Russian Federation, 4Faculty of Physics, Lomonosov Moscow State University, Moscow, Russian Federation
The ability to visualise non-invasively impaired lung ventilation and perfusion caused by lung scarring is important in monitoring recovery of Covid-19 survivors. The hp Xenon-129 imaging modality is currently approved for clinical use in the UK only, however, it has been shown recently that 1H PREFUL methodology can be used to visualise lung perfusion and ventilation in health and disease at 3T whole body scanners. However, 3T scanners may not be available for healthcare in countries with low and middle income, hence PREFUL at 0.5T was used to assess lung ventilation and perfusion in health and Covid-19 disease.
|
|||
1741.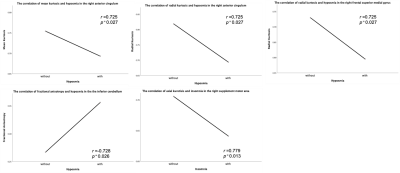 |
Cerebral Microstructural Alteration in Follow-up COVID-19 Patients: A Diffusion Kurtosis Imaging Study
Minhua Yu1, Weiyin Vivian Liu2, Qunfeng Wang3, Dan Xu1, Yumin Liu3, and Haibo Xu1
1Radiology, Zhongnan Hospital of Wuhan University, Wuhan, China, 2MR Research, GE Healthcare, Beijing, China, 3Neurology, Zhongnan Hospital of Wuhan University, Wuhan, China
This study aims to investigate the cerebral microstructural alteration of follow-up recovered COVID-19 (rCOVID-19) patients and explore the corrections of symptoms and microstructure changes. Decreased axial kurtosis (Kax), radial kurtosis (Krad), mean kurtosis (Kmean), mean kurtosis tensor (KTmean) and increased fractional anisotropy (FA) in several brain regions of rCOVID-19 patients indicated demyelination and increased cell membrane permeability of cerebral cortex. Hyposmia was negatively correlated with Kmean and Krad in right anterior cingulum of rCOVID-19 patients, partly explaining the residual olfactory impairment several months after recovery. DKI metrics can help reveal microstructural changes of CNS for rCOVID-19 patients.
|
|||
1742.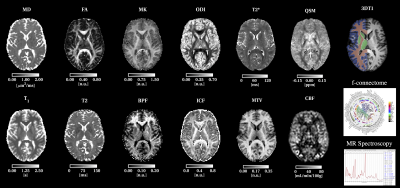 |
Advanced magnetic resonance imaging to study brain tissue alterations in people infected with SARS-COV-2
Claudia A.M. Gandini Wheeler-Kingshott1,2,3, Marios C. Yiannakas1, Janine Makaronidis4,5,6, Ferran Prados7,8, Baris Kanber7, Bhavana S. Solanky1, Marco Battiston1, Jed Wingrove4, Francesco Grussu1,7,9, Gloria Castellazzi10,11, Jonathan Stutters1, James McStravick1, Anita Karsa12,
Rebecca Samson1, Karin Shmueli12, Xavier Golay13, Geoff J. M. Parker1,7, Daniel C. Alexander7, Yael Hacohen1, Egidio D'Angelo2,3, Frederik Barkhof13,14, Carmen Tur1,15, Louis Grandjean16, Olga Ciccarelli1, and Rachel L. Batterham4,5,6
1NMR Research Unit, Queen Square MS Centre, Department of Neuroinflammation, UCL Queen Square Institute of Neurology, Faculty of Brain Sciences, University College London (UCL), London, United Kingdom, 2Department of Brain & Behavioural Sciences, University of Pavia, Pavia, Italy, 3Brain Connectivity Center Research Department, IRCCS Mondino Foundation, Pavia, Italy, 4UCL Centre for Obesity Research, Division of Medicine, University College London (UCL), London, United Kingdom, 5Bariatric Centre for Weight Management and Metabolic Surgery, University College London Hospital (UCLH), London, United Kingdom, 6National Institute of Health Research, UCLH Biomedical Research Centre, London, United Kingdom, 7Centre for Medical Image Computing, University College London (UCL), London, United Kingdom, 8E-Health Center, Universitat Oberta de Catalunya, Barcelona, Spain, 9Radiomics Group, Vall d’Hebron Institute of Oncology, Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain, 10IRCCS Mondino Foundation, Pavia, Italy, 11Department of Electrical, Computer and Biomedical Engineering, University of Pavia, Pavia, Italy, 12Department of Medical Physics & Biomedical Engineering, University College London (UCL), London, United Kingdom, 13Department of Brain Repair & Rehabilitation, University College London (UCL), London, United Kingdom, 14Radiology, VU Medical Centre Amsterdam, Amsterdam, Netherlands, 15Neurology-Neuroimmunology Department, Multiple Sclerosis Centre of Catalonia (Cemcat), Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain, 16Department of Infection, Inflammation and Immunity, Institute of Child Health, University College London (UCL), London, United Kingdom
COVID-19 has now been associated with neurological symptoms, but the pathogenesis of such symptoms is unknown. Advanced quantitative MRI can provide information on alterations of brain tissue properties beyond clinically identifiable lesions. We developed a novel comprehensive scanning protocol and highly automated analysis pipeline to compare brain structure and function in people who were exposed to SARS-COV-2 infection against people who were not. Initial findings indicate that COVID-19 alters white matter microstructure and brain metabolism.
|
|||
1743.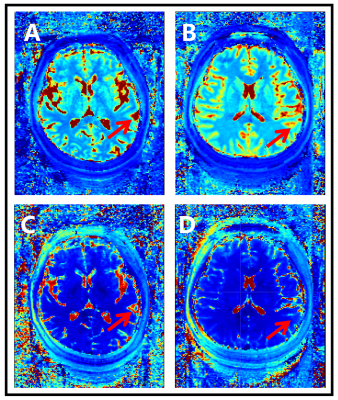 |
Magnetic resonance fingerprinting in two-month-recovered COVID-19 patients
Yaping Wu1, Xianchang Zhang2, Yu Shen1, Yan Bai1, Wei Wei1, Congyu Liao3, and Meiyun Wang1
1Department of Medical Imaging, Henan Provincial People’s Hospital & the People’s Hospital of Zhengzhou University, Zhengzhou, China, 2MR Collaboration, Siemens Healthcare Ltd., Beijing, China, 3Athinoula A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States
This study investigated the utility of magnetic resonance fingerprinting (MRF) to detect potential brain changes in recovered COVID-19 patients. MRF T1 and T2 maps of the brains of 8 recovered COVID-19 patients and 8 volunteers were non-linearly normalized into the MNI space to explore the differences between the groups using whole-brain analysis. COVID-19 patients had significantly lower T1 and T2 values in the left superior temporal gyrus, near the hub for the olfaction and gustation systems, and other brain areas. Our findings suggest that SARS-CoV-2 may widely affect the neurological system, and the effect persisted after more than two months.
|
|||
1744.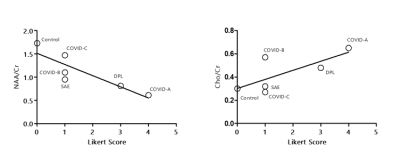 |
Brain Metabolic Changes in COVID-19 Patients: Preliminary Observations.
Akila Weerasekera1,2, Otto Rapalino1, Sarah J Moum1, Katharina Eikermann-Haerter1, Brian Edlow3, David Fischer1, Angel Torrado-Carvajal1,4, Marco L Loggia1, Shibani Mukerji3, Pamela L Schaefer1, Ramon Gilberto Gonzalez1, Michael Lev1, and Eva-Maria Ratai1
1Department of Radiology, Massachusetts General Hospital and Harvard Medical School, Boston, MA, United States, 22A. A. Martinos Center for Biomedical Imaging, Boston, MA, United States, 3Neurology, Massachusetts General Hospital and Harvard Medical School, Boston, MA, United States, 4Medical Image Analysis and Biometry Laboratory, Universidad Rey Juan Carlos, Madrid, Spain
Here we report for the first time metabolic abnormalities in white matter lesions of COVID-19 patients using MR-spectroscopic imaging. The study compares metabolic changes in COVID-19 patients to those seen in other encephalopathies and a normal control case. Findings include NAA reduction indicating neuronal injury/loss, and choline and myo-inositol elevation indicating demyelination and neuroinflammation, respectively. One COVID-19 patient exhibited pronounced lactate elevation consistent with "silent hypoxia". Other factors may be involved considering the degree of metabolic changes seen in these patients when compared to other COVID-19 cases without similar white matter changes as well as other white matter disorders.
|
|||
1745. |
Towards to quantitative evaluation of brain damages in recovered COVID-19 patients using Synthetic MRI
Xie Qing1, Niu Shanshan1, Liao Jianwei1, Li Yingqin1, Qian Long2, Zhang Yaqin1, and Li Shaolin1
1Department of Radiology, the Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, Guangdong, China, 2MR Research, GE Healthcare, Beijing, China
Increasing evidences support that SARS-CoV-2 can invade the central nervous system (CNS) and damage neuronal cells. However, there is no study to unravel the brain microstructural changes associated with SARS-CoV-2. Synthetic MRI provides T1 and T2 mapping, which could quantitatively evaluate the tissue microstructures. In current study, our goal is to assess the microstructural involvement of gray matter in recovered COVID-19 patients using Synthetic MRI. Our results indicated that the microstructure component of gray matter is disrupted in recovered COVID-19 patients, which provided the evidence of CNS damages.
|
|||
1746.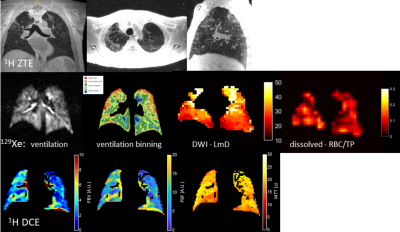 |
Imaging lung structure and function in acute COVID-19 patients with 129Xe and 1H MRI
Guilhem J Collier1, Jody Bray1, Ho-Fung Chan1, Paul J.C. Hughes1, James A Eaden1, Laurie J Smith1, Helen Marshall1, David J Capener1, Leanne Armstrong1, Alberto M Biancardi1, Madhwesha R Rao1, Graham Norquay1, Oliver Rodgers1,
Andy J Swift1, Smitha Rajaram2, Fergus Gleeson3, James T Grist3, Gary H Mills4, James Meiring2, Lisa Watson2, Paul J Collini4, Roger Thompson4, Rod Lawson2, and Jim M Wild1
1POLARIS, Department of Infection, Immunity & Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Sheffield teaching hospitals, NHS Foundation TRUST, Sheffield, United Kingdom, 3Department of Radiology, Oxford NHS Foundation Trust, Oxford, United Kingdom, 4Department of Infection, Immunity & Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom
We assessed the sensitivity of a comprehensive multi-nuclear lung function-structure imaging protocol to acute changes in the lungs of patients admitted to hospital with COVID-19 lung infection. Dissolved 129Xe spectroscopic imaging and DCE 1H perfusion MRI indicate impaired gas transfer related to diffusion and microvascular perfusion limitation, whilst 129Xe ventilation MRI and 129Xe DWI indicate fairly homogenous lung ventilation and airway microstructure, apart from in areas showing clear structural abnormality on UTE/ZTE imaging (residual ground glass opacity or consolidation). The findings provide quantitative regional insight in to why patients suffer from severe breathlessness despite their lung ventilation appearing near normal.
|
|||
1747.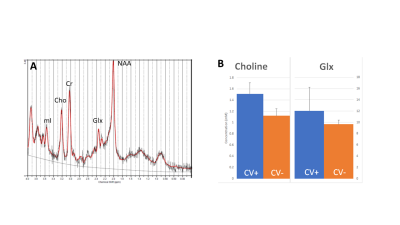 |
Magnetic Resonance Spectroscopy of Long COVID: Preliminary Study
Alexander Lin1, Min Zhou2, Huijun Liao1, Eduardo Coello1, and Jong-Woo Lee3
1Center for Clinical Spectroscopy, Brigham and Women's Hospital, Boston, MA, United States, 2Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, 3Department of Neurology, Brigham and Women's Hospital, Boston, MA, United States
The goal of this study was to measure brain metabolites in patients recovered from COVID-19 to examine the chronic effects of COVID, also known as long COVID, which have been shown to have neurological effects. Spectroscopy in the cingulate gyrus revealed increased choline and glutamate/glutamine which may be reflective of neuroinflammatory changes due to long COVID.
|
|||
1748.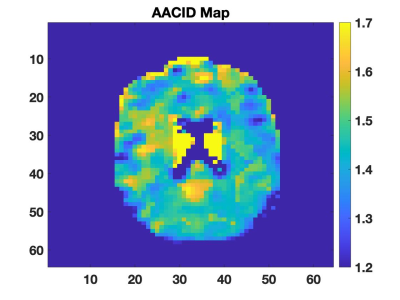 |
Long-term cognitive and neurological Effects of COVID-19 Illness detected by 7T MRI
Helma Heidari1,2, Stephanie Handsor3, Koula Pantazopoulos4, Lauryn Richardson4, Kristy Coleman4, Michael Silverman5, Erin Spicer3, Stephen Pasternak4,6, Luciano Sposato6, Doug Fraser7, Anthony Tang8, Ravi S. Menon1,2, Corey Baron1,2,
Michael Jurkiewicz9, Elizabeth Finger4,6, Marko Mrkobrada3, Megan Devlin3, and Robert Bartha1,2
1Robarts research Institute, London, ON, Canada, 2Medical Biophysics, The University of Western Ontario, London, ON, Canada, 3Internal Medicine, The University of Western Ontario, London, ON, Canada, 4Parkwood Institute, London, ON, Canada, 5Infectious Diseases, The University of Western Ontario, London, ON, Canada, 6Clinical Neurological Sciences, The University of Western Ontario, London, ON, Canada, 7Paediatric Critical Care, The University of Western Ontario, London, ON, Canada, 8Medicine, The University of Western Ontario, London, ON, Canada, 9Medical Imaging, The University of Western Ontario, London, ON, Canada
Evidences support that the new SARS-Cov2 virus has neurological consequences in patients. Using the high resolution and sensitivity of 7T MRI, this study will determine if prolonged cognitive and neurological symptoms in patients recovered from COVID-19 illness are related to brain imaging findings. Six patients with neurological symptoms during their illness and with no respiratory symptoms for at least one month have been recruited to date. Advanced 7T MRI including susceptibility weighted imaging, diffusion tensor imaging, and chemical exchange saturation transfer imaging has been successfully acquired in four subjects with patient recruitment ongoing.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.