Digital Poster
Advances in Treatment of Neurologic Disorders
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
1852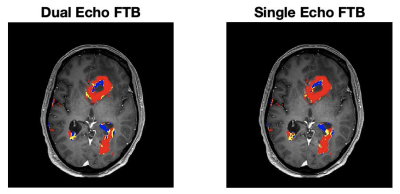 |
32 | Identification of a single-dose, dual-echo based CBV threshold for fractional tumor burden mapping in recurrent glioblastoma
Aliya Anil1, Ashely M Stokes1, Renee Chao1, Leland Hu2, Lea Alhilali3, John P Karis3, Laura C Bell4, and C Chad Quarles1
1Division of Neuroimaging Research and Barrow Neuroimaging Innovation Center, Barrow Neurological Institute, Phoenix, AZ, United States, 2Mayo Clinic Arizona, Phoenix, AZ, United States, 3Southwest Neuroimaging at Barrow Neurological Institute, Phoeix, AZ, United States, 4Genentech, South Francisco, CA, United States Reliable differentiation of tumor recurrence and treatment effects in glioblastoma patients is still a prevailing challenge. The purpose of this study is to identify the optimal threshold for generating fractional tumor burden (FTB) maps derived from single-dose, dual-echo based standardized relative cerebral blood volume measurements. To establish the threshold, dual-echo data was compared to the well-validated, double-dose single echo standardized FTB map. In summary, with the optimized threshold, the single-dose, dual-echo approach yielded FTB maps that strongly agreed with the reference standard, providing a compelling option for clinical use. |
||
1853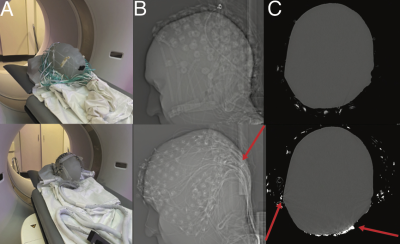 |
33 | Improving multimodal imaging with an MR-compatible EEG net: the R-Net-MR-IT
Nina Fultz1,2,3, Hongbae Jeong1, Stephanie D. Williams1,3, Daniel E.P. Gomez1,3, Beverly Setzer1,3, Tracy Warbrick4, Manfred Jaschke4, Giorgio Bonmassar1, and Laura D. Lewis1,3
1Athinoula A. Martinos Center for Biomedical Engineering, Charlestown, MA, United States, 2Department of Neuroscience, University of Copenhagen, Copenhagen, Denmark, 3Department of Engineering, Boston University, Boston, MA, United States, 4Brain Products GmbH, Gilching, Germany
EEG provides valuable clinical information, but EEG nets produce artifacts in MRI and CT images, preventing these modalities from being combined in typical clinical practice. We tested whether a new MR-compatible EEG net, called the R-Net-MR-IT, could produce high-quality clinical and research images. We assessed image quality in CT and MR images on a phantom with a conventional net, R-Net-MR-IT, and with no net. We then performed the same comparison in humans, as well as fMRI scans. Our results show that the R-Net-MR-IT enables acquisition of high quality CT and MR images, with minimal artifact from EEG hardware.
|
||
1854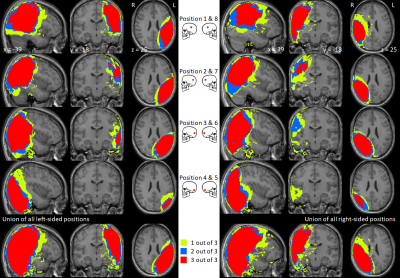 |
34 | MRI of individuals with cochlear implants: surgical planning, current practice, success rates, and stakeholder opinions
Rebecca Susan Dewey1,2,3, Robert Dineen1,4,5, Matthew Clemence6, Olivier Dick7, Richard Bowtell1, and Pádraig Kitterick8
1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2Hearing Sciences, Division of Mental Health and Clinical Neurosciences, School of Medicine, University of Nottingham, Nottingham, United Kingdom, 3Hearing Theme, NIHR Nottingham Biomedical Research Centre, Nottingham, United Kingdom, 4Imaging Theme, NIHR Nottingham Biomedical Research Centre, Nottingham, United Kingdom, 5Radiological Sciences, Division of Mental Health and Clinical Neurosciences, School of Medicine, University of Nottingham, Nottingham, United Kingdom, 6Philips Healthcare, Best, Netherlands, 7Radiology Department, Queens Medical Centre, Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom, 8National Acoustic Laboratories, Sydney, Australia
A cochlear implant (CI) contains a magnet implanted under the scalp. MRI of CI users is associated with safety concerns, significant discomfort, and image distortion. A CI placed under a swimming cap is a feasible tool for observing the effect of CI location on image usability within a single subject and potentially informing surgical planning. 35-70% of radiological features in the head were deemed unaffected by the implant. Online survey results highlight the need for consistent publication of clear, succinct, and standardised information for healthcare professionals and CI users. CI user consultation is scarce, meaning their views are often neglected.
|
||
1855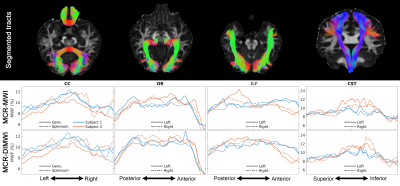 |
35 | Test-retest repeatability study of multi-compartment relaxometry for myelin water imaging (MCR-MWI)
Kwok-Shing Chan1, Maxime Chamberland1, and José P Marques1
1Donders Institute for Brain, Cognition and Behaviour, Nijmegen, Netherlands In this study, we evaluate the test-retest repeatability of the recently developed multi-compartment relaxometry method for myelin water imaging (MCR-MWI). Cross-protocol repeatability is also studied using 3 GRE protocols with different echo spacing and TR. Good cross-session and cross-protocol repeatability is observed for MCR-MWI. Additionally, tissue parameters along 8 major white matter bundles are studied, and myelin water fraction is the most robust tissue parameter across various protocol settings. |
||
1856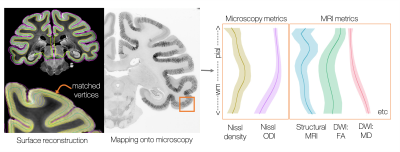 |
36 | The BigMac dataset: interconnecting MR signals with microstructure profiles in the cortex
Amy FD Howard1, Istvan N Huszar1, Michiel Cottaar1, Greg Daubney2, Alexandre A Khrapitchev3, Rogier B Mars1,4, Jeroen Mollink1, Lea Roumazeilles2, Connor Scott5, Adele Smart5, Jerome Sallet2, Saad Jbabdi1, and Karla L Miller1
1Wellcome Centre for Integrative Neuroimaging (FMRIB), Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom, 2Wellcome Centre for Integrative Neuroimaging, Experimental Psychology, Medical Sciences Division, University of Oxford, Oxford, United Kingdom, 3MRC Oxford Institute for Radiation Oncology, Department of Oncology, University of Oxford, Oxford, United Kingdom, 4Donders Institute for Brain, Cognition and Behaviour, Radboud University Nijmegen, Nijmegen, Netherlands, 5Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom Microscopy data can provide detailed descriptions of how cortical microstructure varies across the brain. However, the relationship between cortical microstructure and MRI signals remains relatively unexplored. Here we develop a pipeline to extract cortical profiles from co-registered MRI and microscopy data in the BigMac dataset. We compare cortical profiles of cell density and microstructural dispersion from Nissl-stained histology slides with matched profiles from structural and diffusion MRI. Using CCA we find modes of microstructure variation common to microscopy and structural MRI, but not diffusion, indicating variable sensitivity of the MR metrics to brain-wide variations in Nissl-stained cytoarchitecture. |
||
1857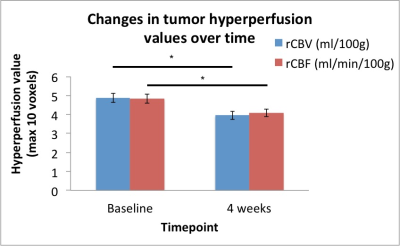 |
37 | Anti-angiogenic therapy in recurrent glioblastoma uncouples tumor hyperperfusion measures from spectroscopic measures of Lac/c-Cr
Pratik Talati1,2, Benjamin Chun2, Patrick Clark2, Anthony Ranasinghe2, Mohamed E. El-Abtah2, Melanie Fu2, Julian He3, Otto Rapalino4, R. Gilberto Gonzalez4, Jorg Dietrich5, Elizabeth R. Gerstner5, and Eva-Maria Ratai2
1Neurosurgery, Massachusetts General Hospital, Boston, MA, United States, 2A. A. Martinos Center for Biomedical Imaging, Charlestown, MA, United States, 3Radiology, Massachusetts General Hospital, Boston, MA, United States, 4Neuroradiology, Massachusetts General Hospital, Boston, MA, United States, 5Neuro-oncology, Massachusetts General Hospital, Boston, MA, United States
Patients with recurrent glioblastoma (rGBM) are often started on anti-angiogenic therapy, making it challenging to determine disease progression with standard MR methods. We performed a prospective analysis on 14 patients with rGBM utilizing MR spectroscopy and DSC-perfusion imaging to investigate metabolic changes before and 4 weeks after anti-angiogenic therapy. We found that anti-angiogenic therapy significantly decreases relative tumor hyperperfusion values of CBV and CBF and uncouples a correlation between CBV and CBF with Lac/c-Cr. Baseline hyperperfusion values can stratify longer-term from shorter-term survivors at nine months. Further investigation into the early stages of anti-angiogenic therapy are warranted.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.