Digital Poster
Modeling, Analysis & Evaluation II
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
2785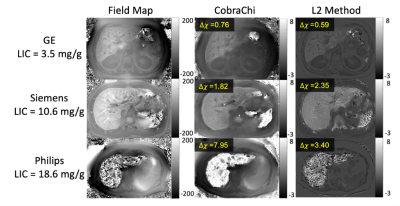 |
53 | Multi-center, Multi-vendor evaluation of quantitative susceptibility mapping for quantification of liver iron
Collin J. Buelo1,2, Ruiyang Zhao1,2, Julia V. Velikina1, Steffen Bollmann3, Ante Zhu4, Qing Yuan5, Mounes Aliyari Ghasabeh6, Stefan Ruschke7, Dimitrios C. Karampinos7, David T. Harris1, Ryan J. Mattison8, Michael R. Jeng9, Ivan Pedrosa5, Ihab R. Kamel5, Shreyas Vasanawala10, Takeshi Yokoo5,11, Scott B. Reeder1,2,8,12,13, and Diego Hernando1,2
1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 33School of Information Technology and Electrical Engineering, The University of Queensland, Brisbane, Australia, 4GE Global Research, Niskayuna, NY, United States, 5Radiology, University of Texas Southwestern Medical Center, Dallas, TX, United States, 6Radiology, The Johns Hopkins University, Baltimore, MD, United States, 7Department of Diagnostic and Interventional Radiology, Technical University of Munich, Munich, Germany, 8Medicine, University of Wisconsin-Madison, Madison, WI, United States, 9Pediatrics - Hematology & Oncology, Stanford University, Palo Alto, CA, United States, 10Radiology, Stanford University, Palo Alto, CA, United States, 11Advanced Imaging Research Center, University of Texas Southwestern Medical Center, Dallas, TX, United States, 12Department of Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 13Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
Quantitative susceptibility mapping (QSM) of the liver is an emerging method to quantify liver iron concentration (LIC). Multiple new methods have recently been introduced for QSM in the liver. These methods include CobraChi, a deep learning-based method, as well as an L2-optimization based method. This work evaluates the performance of these liver QSM methods across multiple centers and MRI vendors.
|
||
2786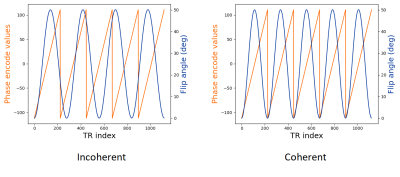 |
54 | Non-steady-state sequences for multi-parametric MRI need to be evaluated in the context of gradient-encoding
Miha Fuderer1,2, Oscar van der Heide1, Hongyan Liu1, Cornelis A.T. van den Berg1, and Alessandro Sbrizzi1
1Computational Imaging Group for MR Diagnostics and Therapy, Center for Image Sciences, University Medical Center Utrecht, Utrecht, Netherlands, 2Department of Radiology, Division of Imaging and Oncology, University Medical Center Utrecht, Utrecht, Netherlands
In non-steady-state multi-parametric quantitative MRI (e.g. MR-STAT or MR Fingerprinting (MRF)), it is a non-trivial task to devise good sequences of time-varying flip angles. Recent work addresses this issue, albeit assuming a single-voxel approach, i.e. the k-space encoding is not taken into account when optimizing. In this work we show, using examples from MR-STAT reconstructions and using a Cramer-Rao based BLAKJac analysis, that two apparently similar sequences can have vastly different outcomes when applied in an actual (2-dimensional) measurement setup - showing that the context of encoding is very relevant.
|
||
2787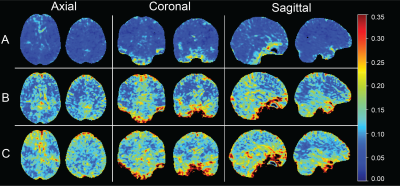 |
55 | APT-CEST Scan-Rescan Reproducibility in Healthy Volunteers and Brain Glioma Patients at 3 Tesla
Ivar J.H.G. Wamelink1, Beatriz Padrela1, Joost P.A. Kuijer1, Yi Zhang2, Frederik Barkhof1,3, Henk J.M.M. Mutsaerts1, Elsmarieke van de Giessen1, and Vera C. Keil1
1Department of Radiology and Nuclear Medicine, Vrije Universiteit Amsterdam Medisch Centrum, Amsterdam, Netherlands, 2Department of Biomedical Engineering, Key Laboratory for Biomedical Engineering of Ministry of Education, Department of Biomedical Engineering, College of Biomedical Engineering & Instrument Science, Zhejiang University, Hangzhou, Zhejiang, China, 3UCL Institutes of Neurology and Healthcare Engineering, London, United Kingdom Amide proton transfer (APT) chemical exchange saturation transfer (CEST) MRI is a potentially useful clinical technique to image brain tumors, but its reproducibility was not yet investigated in detail. Our 3T scan-rescan protocol on volunteers and glioma patients revealed high within-session and slightly lower in-between-session and between-day reproducibility, with highest reproducibility occipitally and centrally in the brain and lowest at the skull base. The within-session reproducibility for patients was also good, both intratumoral and extratumoral. These results show that APT-CEST at 3T MRI renders reproducible values allowing for clinical monitoring of metabolic brain tumors. |
||
2788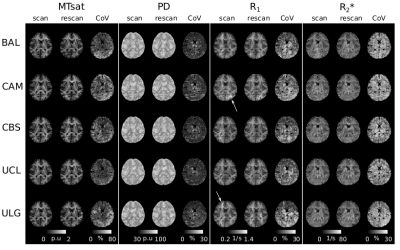 |
56 | Repeatability of ultra-high-resolution Multi-Parametric Mapping across five 7T sites
siya sherif1, Ali Aghaeifar2,3, Kerrin Pine4, Belinda Ding5, Maryam Seif6, Evelyne Balteau1, Daniel Nanz7,8, Christine Bastin1, Eric Salmon1,9, Pierre Maquet1,9, Gilles Vandewalle1, Christopher T Rodgers 5, Patrick Freund6, Nikolaus Weiskopf4,10, Christophe Phillips1,11, and Martina F Callaghan3
1GIGA-Cyclotron Research Centre - In Vivo Imaging, University of Liège, Liège, Belgium, 2MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom, 3Wellcome Centre for Human Neuroimaging, University College London, London, United Kingdom, 4Department of Neurophysics, Max Planck Institute for Human Cognitive and Brain Sciences, Leipzig, Germany, 5Wolfson Brain Imaging Centre, University of Cambridge, Cambridge, United Kingdom, 6Spinal cord injury Center, University of Zurich, Zurich, Switzerland, 7Swiss Center for Musculoskeletal Imaging, Zurich, Switzerland, 8University of Zurich, Zurich, Switzerland, 9Department of Neurology, University Hospital of Liège, Liège, Belgium, 10Felix Bloch Institute for Solid State Physics, Leipzig University, Leipzig, Germany, 11GIGA - In Silico Medicine, University of Liège, Liège, Belgium
Repeatability is key to the utility of quantitative MRI, which promises standardised measures with biological relevance. Here we tested a candidate ultra-high resolution (0.6mm isotropic) multi-parameter mapping protocol at five 7T sites. Repeatability was good, with B0 and B1+ field inhomogeneities being the limiting factor. MTsat had the lowest repeatability and PD the highest. R1 and R2* were intermediate. Repeatability was also lowest in temporal and occipital cortices. These observations were consistent across sites.
|
||
2789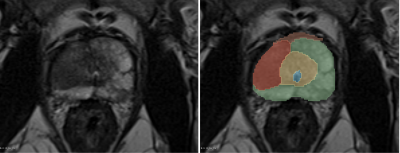 |
57 | Test-retest repeatability of radiomic features derived from T2w MRI in prostate cancer patients
Barbara Daria Wichtmann1, Steffen Albert2, Daniel Pinto dos Santos3, Ulrike Irmgard Attenberger1, and Bettina Baessler4
1Department of Diagnostic and Interventional Radiology, University Hospital Bonn, Bonn, Germany, 2Computer Assisted Clinical Medicine, Mannheim Institute for Intelligent Systems in Medicine, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany, 3Department of Radiology, University Hospital Cologne, Cologne, Germany, 4Institute of Diagnostic and Interventional Radiology, University Hospital Wuerzburg, Wuerzburg, Germany
Radiomics enables the extraction of quantitative features from medical images, potentially augmenting the characterization of healthy and diseased tissue. Before these features can be routinely used as biomarkers in clinical practice, however, their repeatability and reproducibility must be ensured. This study seeks to investigate feature repeatability in an in-vivo, clinical test-retest dataset of prostate cancer patients. Our results show that the majority (71.8%) of radiomic features extracted from in-vivo, clinical T2-weighted images was not repeatable, emphasizing the need for repeatability and reproducibility studies.
|
||
2790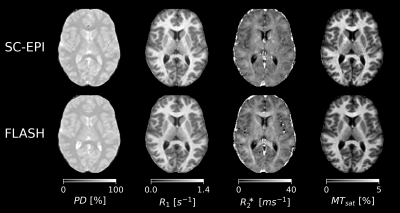 |
58 | Reproducibility of rapid quantitative multiparameter mapping using skipped-CAIPI 3D-EPI
Difei Wang1, Rüdiger Stirnberg1, and Tony Stöcker1,2
1German Center for Neurodegenerative Diseases (DZNE), Bonn, Germany, 2Department of Physics and Astronomy, University of Bonn, Bonn, Germany
We investigated the reproducibility of multiparameter mapping (MPM) using multi-echo skipped-CAIPI 3D-EPI at 3T. Compared to >15 minutes of FLASH-MPM, EPI-MPM under 3 minutes achieved considerably high repeatability. In only one fifth of the total scan time of FLASH, the resulting CoVs of EPI were only 1.2-2.2 times larger than FLASH for R1, PD and MTsat, while the CoV of EPI for R2* was even smaller. Minor differences of the observed parameter estimates can be attributed to the intrinsic difference between EPI and FLASH sequence timing.
|
||
2791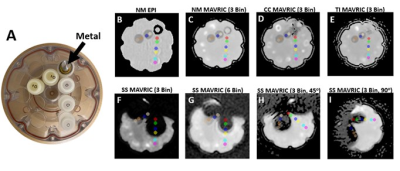 |
59 | Quantitative Assessment of Diffusion Weighted Imaging Near Metal Implants
John P. Neri1, Matthew F. Koff1, Kevin M. Koch2, and Ek T. Tan1
1Hospital for Special Surgery, New York, NY, United States, 2Medical College of Wisconsin, Milwaukee, WI, United States
Conventional echo-planar imaging (EPI) DWI suffers from substantial artifact when imaging orthopedic hardware. DWI with multi-acquisition with variable resonance image combination (MAVRIC) can reduce susceptibility artifact around metal implants. The purpose of this work was to evaluate the quantitative accuracy of DWI-MAVRIC near metal components using a diffusion phantom. DWI-MAVRIC sequences were acquired in the presence of no metal, cobalt-chromium, titanium, and stainless steel. It was found that DWI-MAVRIC can accurately measure apparent diffusion coefficient (ADC) in the presence of metal. Among tested metals, stainless steel creates the greatest artifact that prevented the acquisition of accurate ADC data.
|
||
2792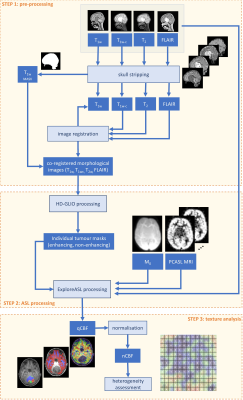 |
60 | Heterogeneity of ASL perfusion MRI in low-grade paediatric glioma as imaging biomarker to assess treatment effect
Lejla Alic1, Sanneke C Willekens1,2, Henk-Jan M.M. Mutsaerts2, Jan Petr3, Netteke A.Y.N. Schouten-van Meeteren4,5, Maarten M.H. Lequin6, and Evita E.C. Wiegers2
1Magnetic Detection & Imaging Group, University of Twente, Enschede, Netherlands, 2Department of Radiology, University Medical Center Utrecht, Utrecht, Netherlands, 3Helmholtz-Zentrum Dresden-Rossendorf, Institute for Radiopharmaceutical Cancer Research, Dresden, Germany, 4Radiology and Nuclear Medicine, Amsterdam Neuroscience, Amsterdam, Netherlands, 5Department of Neuro-oncology, Princess Máxima Centre, Utrecht, Netherlands, 6Radiology, University Medical Center Utrecht, Utrecht, Netherlands
ASL-MRI is reported as an option to assess potentially heterogeneous physiological processes important for tumour treatment. Therefore, we explored the heterogeneity in normalised CBF as an imaging biomarker for assessment of treatment effect in pLGG. There is a noticeable effect of chemotherapy observed as a change in texture of healthy appearing brain tissue. A high difference in texture between treated and non-treated patients for non-enhancing tumour part is observed, suggesting that texture, based on co-occurrence matrices, is suitable as an imaging biomarker for assessment of treatment effect in pLGG.
|
||
2793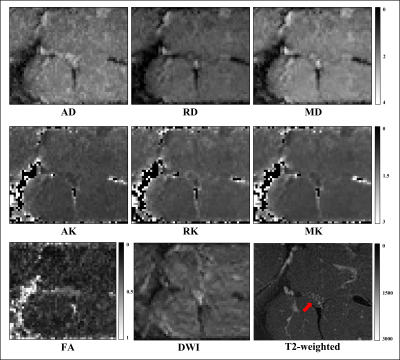 |
61 | Reduced field-of-view multi-shell DWI of the sciatic nerve: A reproducibility assessment Video Permission Withheld
Ratthaporn Boonsuth1, Rebecca S Samson1, Francesco Grussu1,2, Marco Battiston1, Torben Schneider3, Masami Yoneyama4, Ferran Prados1,5,6, Carmen Tur1,7, Sara Collorone1, Rosa Cortese1, Claudia AM Gandini Wheeler-Kingshott1,8,9, and Marios C Yiannakas1
1NMR Research Unit, Queen Square MS Centre, Department of Neuroinflammation, UCL Queen Square Institute of Neurology, University College London, London, United Kingdom, 2Radiomics Group, Vall d’Hebron Institute of Oncology, Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain, 3Philips Healthcare, Guildford, Surrey, United Kingdom, 4Philips Japan, Minatoku, Tokyo, Japan, 5Centre for Medical Image Computing, Department of Medical Physics and Biomedical Engineering, University College London, London, United Kingdom, 6E-Heath Centre, Universitat Oberta de Catalunya, Barcelona, Spain, 7Multiple Sclerosis Centre of Catalonia (Cemcat), Vall d’Hebron Institute of Research, Vall d'Hebron Barcelona Hospital Campus, Barcelona, Spain, 8Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy, 9Brain Connectivity Research Centre, IRCCS Mondino Foundation, Pavia, Italy
Advanced diffusion-weighted imaging (DWI) methods are powerful diagnostic and research tools when applied in the central nervous system (CNS). However, the use of DWI methods to study individual nerves outside the CNS in vivo, such as the sciatic nerve, has been hampered by a number of technical challenges. In this study, we explore the feasibility of acquiring multi-shell DWI metrics in the sciatic nerve using reduced field-of-view echo planar imaging and report results from a reproducibility assessment in in healthy controls.
|
||
2794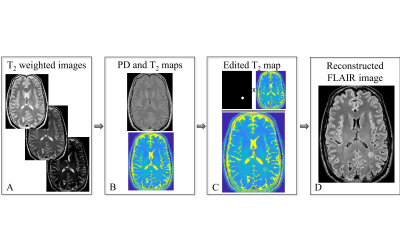 |
62 | Psychophysical evaluation of radiologic vs. deep-learning based identification of multiple sclerosis brain lesions
Chen Solomon1, Omer Shmueli1, Tamar Blumenfeld-Katzir1, Dvir Radunsky1, Noam Omer1, Neta Stern1, Shai Shrot2,3, Moti Salti4,5, Hayit Greenspan1, and Noam Ben-Eliezer6,7
1Biomedical Engineering, Tel Aviv University, Tel Aviv, Israel, 2Department of Diagnostic Imaging, Sheba Medical Center, Ramat Gan, Israel, 3Tel Aviv University, Tel Aviv, Israel, 4Brain Imaging Research Center, Soroka Medical Center, Beer Sheva, Israel, 5University Medical Center, Ben Gurion University, Beer Sheva, Israel, 6Center for Advanced Imaging Innovation and Research (CAI2R), New-York University Langone Medical Center, New York, NY, United States, 7Sagol School of Neuroscience, Tel Aviv University, Tel Aviv, Israel
Computer assisted detection (CAD) of pathology in MRI scans may provide higher sensitivity to tissue changes. We present rigorous comparison of CAD vs. conventional radiologic evaluation of multiple sclerosis (MS) lesions. A psychophysical experiment was performed, where radiologists and a deep neural-network were asked to detect artificial MS lesions, synthetically simulated on T2-weighted FLAIR images, and at 8 levels of severity. Odds ratio analysis indicated that the human vision is less sensitive to low-severity lesions. This suggests that CAD can improve early detection of tissue abnormalities in the brain.
|
||
2795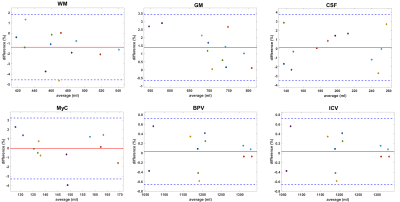 |
63 | Test-retest and inter-vendor variability of brain segmentation using 3D synthetic MRI in volunteers at 3T
Maarten Naeyaert1, Tim Vanderhasselt1, and Hubert Raeymaekers1
1Radiology, Universitair Ziekenhuis Brussel, Brussels, Belgium
Six volunteers were scanned two times on two different 3T scanners (GE, Philips) using the 3D-QALAS sequence. The intracranial and brain parenchymal volume and myelin content were determined and the brain segmented in cerebrospinal fluid and white and grey matter using synthetic MRI. Bland-Altman plots, Dice coefficient and coefficient of variation indicate that the test-retest variability is very small, but there is an inter-vendor bias for CSF, GM and WM. MyC, BPV and ICV have only a very limited inter-vendor bias. At least for GM and BPV, the expected inter-scanner variation, besides the bias, is below the clinically relevant threshold.
|
||
2796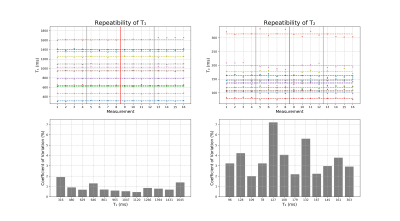 |
64 | Repeatability and accuracy of MR-STAT quantitative T1 and T2 measurements
Oscar van der Heide1,2, Miha Fuderer1,2, Hongyan Liu1,2, Cornelis A.T. van den Berg1,2, and Alessandro Sbrizzi1,2
1Computational Imaging Group for MR Diagnostics and Therapy, Center for Image Sciences, University Medical Center Utrecht, Utrecht, Netherlands, 2Department of Radiology, Division of Imaging and Oncology, University Medical Center Utrecht, Utrecht, Netherlands
MR-STAT is a quantitative MRI technique that obtains multiple tissue parameter maps (e.g. T1, T2) from a single, short scan. In this study we perform an accuracy and repeatability study of MR-STAT using a Cartesian FISP-based sequence by repeatedly scanning Eurospin gel tubes and comparing the results against reference measurements. We observe coefficients of variation between 0.5 % and 1.5 % for T1 and between 2.0 % and 7.2 % for T2. The mean relative errors as compared to the reference measurements are -1.5 % for T1 and 5.8 % for T2.
|
||
2797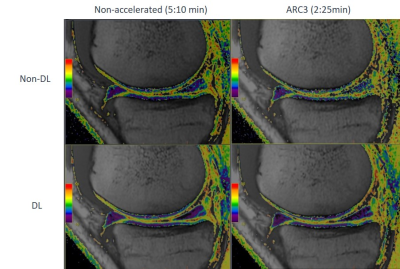 |
65 | Quantitative & qualitative evaluation of accelerated T2 mapping technique using Deep Learning reconstruction in knee cartilage
Laura Carretero1,2, Maggie Fung3, Pablo García-Polo1, Daniel Litwiller4, Marc Lebel5, Graeme C McKinnon6, and Mario Padrón7
1GE Healthcare, Madrid, Spain, 2Rey Juan Carlos University, Madrid, Spain, 3GE Healthcare, New York, NY, United States, 4GE Healthcare, Colorado, CO, United States, 5GE Healthcare, Calgary, AB, Canada, 6GE Healthcare, Waukesha, WI, United States, 7Clínica Cemtro, Madrid, Spain MRI-based cartilage imaging shows biochemical and microstructural changes at early stages of osteoarthritis before changes become visible with structural MRI and arthroscopy. However, clinical application of T2 mapping is driven by high variability and suboptimal reproducibility, besides long examination times. The purpose of this study is to accelerate T2 mapping technique and apply a novel DL reconstruction method to develop a fast and robust way to access T2 relaxometry. Phantom and in-vivo testing demonstrated that DL reconstructed accelerated images provide increased consistency compared to conventional reconstruction and implies a great step into an extensive clinical adoption. |
||
2798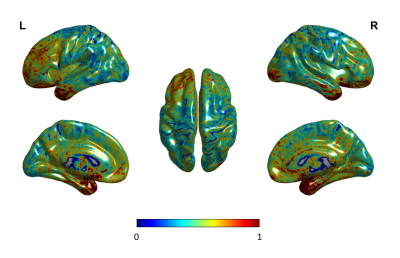 |
66 | Within‐subject reliability of proton density estimation using quantitative magnetic resonance imaging
Karthik R Sreenivasan1, Dietmar Cordes1, Virendra Mishra1, and Le H Hua1
1Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas, NV, United States
New advances in quantitative MRI (qMRI) techniques provide basic MRI properties such as proton density (PD) that can act as a direct surrogate of the tissue integrity in the voxel. PD may help demonstrate differences on an individual level in patients with multiple sclerosis. In this study, we wanted to compare the within-subject reproducibility of qMRI-based PD measures. Variability in the estimated PD was low and fell within the limits for reliability. These results suggest that in-vivo estimates of PD using qMRI are reproducible within the subject in the same scanner and could play a vital role in clinical studies.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.