Digital Poster
Diffuse Liver Disease & Miscellaneous
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
2396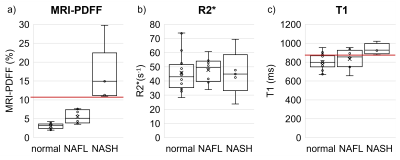 |
25 | PDFF predicts NASH in obese patients without known liver disease
Nikolaos Panagiotopoulos1,2, Danielle Batakis3, Tanya Wolfson4, Rashmi Agni5, Xiaofei Zhang5, Thekla Helene Oechtering1,2, Daiki Tamada1, David T. Harris1, Claude B. Sirlin3, and Scott B. Reeder1,6,7,8,9
1Department of Radiology, University of Wisconsin - Madison, Madison, WI, United States, 2Department of Radiology and Nuclear Medicine, Universität zu Lübeck, Lübeck, Germany, 3Department of Radiology, University of California San Diego, San Diego, CA, United States, 4Computational and Applied Statistics Laboratory, San Diego Supercomputer Center, University of California San Diego, La Jolla, CA, United States, 5Department of Pathology and Laboratory Medicine, University of Wisconsin - Madison, Madison, WI, United States, 6Department of Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 7Department of Medicine, University of Wisconsin - Madison, Madison, WI, United States, 8Department of Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States, 9Department of Emergency Medicine, University of Wisconsin - Madison, Madison, WI, United States Proton density fat fraction (PDFF) is not recognized as a discriminator between nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). However, considering the two-hit theory on the pathogenesis of NASH, we hypothesize that in high-risk individuals without known liver disease, MRI-PDFF may predict the presence of NASH. There is a paucity of data to support this hypothesis. Therefore, we examined the predictive value of MRI-PDFF in 29 obese adults without suspected liver disease. We observed excellent diagnostic performance of MRI-PDFF for detecting NASH (AUC=1). If confirmed during this ongoing study, this would constitute a paradigm change in diagnosis of NASH. |
||
2397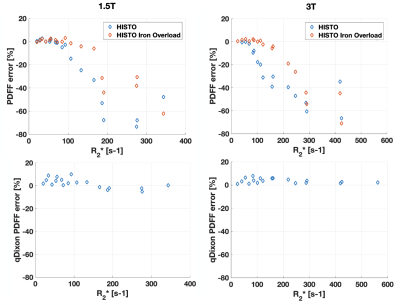 |
26 | Accuracy of a commercial high-speed T2-corrected multi-echo single voxel sequence at 3T as a function of R2* for measurement of liver fat content
Véronique Fortier1,2, Evan McNabb1, Ahmed Mohamed1, Rita Zakarian3, Ives R. Levesque2,3, and Caroline Reinhold1,3,4,5
1Medical Imaging, McGill University Health Center, Montreal, QC, Canada, 2Medical Physics Unit, McGill University, Montreal, QC, Canada, 3Research Institute of McGill University Health Center, Montreal, QC, Canada, 4Diagnostic Radiology, McGill University, Montreal, QC, Canada, 5Montreal Imaging Experts, Inc., Montreal, QC, Canada
Commercial methods for single breath-hold proton density fat fraction (PDFF) quantification in liver can suffer from bias due to the presence of iron. In this work, the PDFF accuracy of a high-speed T2-corrected multi-echo (HISTO) sequence was evaluated at 3T in phantoms at variable R2*, mimicking different iron levels. PDFF errors up to 70% for R2* larger than 150 s-1 were obtained, suggesting that HISTO is unreliable at large liver R2*, as seen with moderate to high iron overload. A Dixon sequence was more accurate at large R2*. Both techniques agreed in patients and phantoms at low PDFF and R2*.
|
||
2398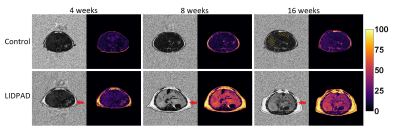 |
27 | Quantitative Dixon imaging to characterise early alterations in liver fat in a novel model of diet-induced MAFLD
Christopher Ball1,2, Zun Siong Low3, Jadegoud Yaligar1, Sanjay Kumar Verma1, Norliza Binte Esmail Sahib3, Hong Sheng Cheng3, Yun Sheng Yip3, Justin Yin Hao Lee3, Debbie Lim3, Walter Wahli3, Harish Poptani2, Nguan Soon Tan3,4, and S. Sendhil Velan1
1Laboratory of Molecular Imaging, Agency for Science Technology and Research (A*STAR), Singapore, Singapore, 2University of Liverpool, Liverpool, United Kingdom, 3Lee Kong Chian School of Medicine, Singapore, Singapore, 4Nanyang Technological University, Singapore, Singapore
A novel diet – LIDPAD – was developed to fulfil the need for a wild-type, diet-induced preclinical model of metabolic associated fatty liver disease that matches all physiologically relevant changes observed during human MAFLD progression.
Stages of MAFLD may be distinguished through MRI and the generation of proton density fat fraction maps. C57BL/6 mice fed on the LIDPAD diet for 4-16 weeks underwent hepatic fat quantification using multi-gradient eight-point Dixon MRI. Physiological changes were assessed through transcriptomic and insulin measurements.
Liver fat increased rapidly, alongside body weight, while transcriptional, metabolic and histological changes mirrored human MAFLD progression.
|
||
2399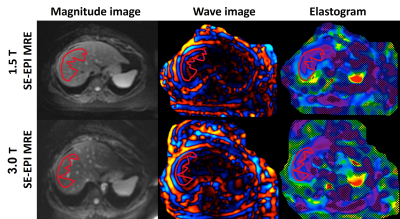 |
28 | Reproducibility of MR Elastography Stiffness Measurements across Field Strength in Obese Adults
Nikolaos Panagiotopoulos1,2, Danielle Batakis3, Tanya Wolfson4, Thekla Helene Oechtering1,2, David T. Harris1, Alan McMillan1,5,6,7, Claude B. Sirlin3, and Scott B. Reeder1,5,6,8,9
1Department of Radiology, University of Wisconsin - Madison, Madison, WI, United States, 2Department of Radiology and Nuclear Medicine, Universität zu Lübeck, Lübeck, Germany, 3Department of Radiology, University of California San Diego, San Diego, CA, United States, 4Computational and Applied Statistics Laboratory, San Diego Supercomputer Center, University of California San Diego, La Jolla, CA, United States, 5Department of Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 6Department of Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States, 7Department of Electrical and Computer Engineering, University of Wisconsin - Madison, Madison, WI, United States, 8Department of Medicine, University of Wisconsin - Madison, Madison, WI, United States, 9Department of Emergency Medicine, University of Wisconsin - Madison, Madison, WI, United States MR elastography (MRE) allows for the quantification of liver stiffness as a quantitative biomarker of liver fibrosis. Between field strength reproducibility has been shown to be high in non-obese populations. Data in obese individuals are limited, however, and obese patients may benefit from early diagnosis as they have an increased risk of liver fibrosis. Therefore, in this work we examined the reproducibility of MRE measurements across field strength in a cohort of 34 obese adults. MRE based liver stiffness measurements were highly reproducible between field strengths. Technical success rate was nearly 100% in this challenging, but relevant population. |
||
2400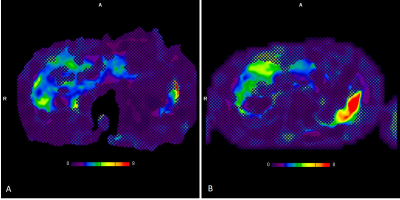 |
29 | MR Elastography-Based Staging of Liver Fibrosis in Fontan Associated liver Disease is Confounded by the Effects of Venous Congestion Video Permission Withheld
Suraj D Serai1, Adarsh Ghosh1, Benjamin J Wilkins2, Anne Marie Cahill1, David M Biko1, Elizabeth Rand3, Jack Rychik4, and David J Goldberg4
1Radiology, The Children's Hospital of Philadelphia, Philadelphia, PA, United States, 2Pathology, The Children's Hospital of Philadelphia, Philadelphia, PA, United States, 3Hepatology, The Children's Hospital of Philadelphia, Philadelphia, PA, United States, 4Cardiology, The Children's Hospital of Philadelphia, Philadelphia, PA, United States
In patients with Fontan, although liver stiffness has been found to increase significantly with age and has been directly correlated with diminished cardiac function, the increased liver stiffness could be influenced by underlying conditions of vascular congestion. The purpose of this study was to compare stiffness as measured by MRE localized by liver biopsy with histological results from biopsy, and to determine the change in MRE defined liver stiffness over time. Our findings have important implications for how liver MRE might be a useful tool in following the progression of liver stiffness longitudinally in patients with Fontan associated liver disease.
|
||
2401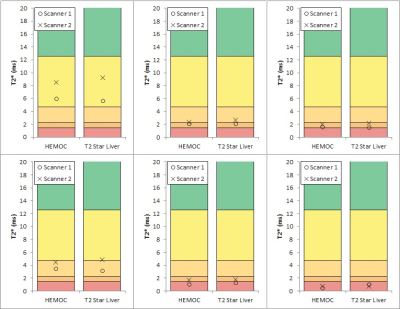 |
30 | Development and Testing of an In-House Phantom to Assess T2*/R2* Relaxometry Measurements of Liver Iron Concentration
Alex Goodall1, Stephen Powell1, Jasmine Lister1, and Andrew Fry1
1Medical Imaging and Medical Physics, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
T2* relaxometry measurements of Liver Iron Concentration are demonstrated to be reliable and reproducible in publications. However, no suitable phantom exists for individual hospitals to validate the accuracy, reliability or precision of their methods. We demonstrate a novel phantom mimicking physiological T2* liver values for this purpose. The accuracy of 2 clinical sequences, reproducibility between 2 scanners and reliability of the phantom was investigated.
|
||
2402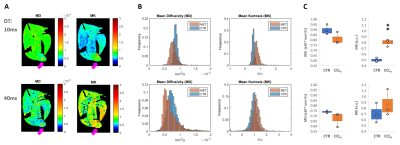 |
31 | Relevance of diffusion time for DKI detection of liver pathology
Rui V Simoes1, Andreia Otake1, Silvia Batista1, Rafael N Henriques1, Bruno Costa-Silva1, and Noam V Shemesh1
1Champalimaud Research, Champalimaud Centre for the Unknown, Lisbon, Portugal
Despite the recent interest in diffusion kurtosis imaging (DKI) for assessing liver pathologies, its added value over more standard diffusion-weighted or diffusion tensor imaging techniques remains to be established. Importantly, mean diffusivity (MD) and mean kurtosis (MK) estimations are strongly dependent on the diffusion time (DT), a parameter generally overlooked in liver DKI studies. Here, we demonstrate ex vivo the relevance of short DT – namely 10 ms rather than 40 ms – for MK detection of liver disease, using two well-described mouse models of liver metastasis and fibrosis.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.