Oral Session
Cerebrovascular: Expanding Limits of Anatomic Resolution & Dynamic Processes
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| 14:30 | 0278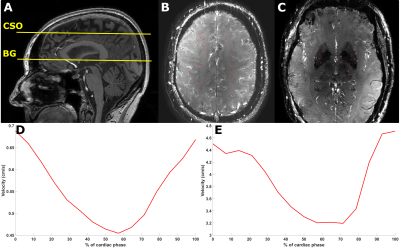 |
Increased Pulsatility Index of Perforating Arteries as Novel 7T Marker in Sporadic Cerebral Small Vessel Disease – Results of ZOOM@SVDs Study.
Stanley D.T. Pham1, Hilde van den Brink2, Tine Arts1, Jeroen C.W. Siero1, Jeroen Hendrikse1, Jaco J.M. Zwanenburg1, and Geert Jan Biessels2
1Radiology, UMC Utrecht, Utrecht, Netherlands, 2Neurology and Neurosurgery, UMC Utrecht, Utrecht, Netherlands
We assessed blood-flow velocity measurements on 7T MRI as a potential disease marker for cerebral small vessel disease (SVD). Two-dimensional phase-contrast velocity measurements were performed in perforating arteries of the basal ganglia (BG) and white matter of the centrum semiovale (CSO) in patients with sporadic SVD and age- and sex-matched controls. Pulsatility index (PI) was significantly higher in the BG, in patients (0.45 [0.41–0.49] vs. 0.36 [0.30–0.41] in controls) (p=0.02). In the CSO, similar number of vessels, mean velocity, and PI were observed between patients and controls. BG pulsatility could be a potential marker for SVD.
|
|
| 14:42 | 0279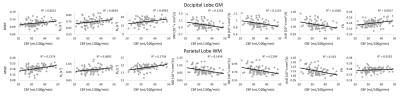 |
Cerebral blood flow is associated with cerebral microstructural integrity in normative aging
Curtis Gregory Triebswetter (Co-Author)1, Matthew Kiely (Co-Author)1, Zhaoyuan Gong1, Maryam H. Alsameen1, and Mustapha Bouhrara1
1National Institute on Aging, Baltimore, MD, United States
Maintenance of cerebral tissue homeostasis is particularly sensitive to deficits in cerebral blood flow (CBF) and concomitant hypoxia and hypoglycemia. However, little work has been conducted to investigate the potential association between deficits in CBF and deterioration of brain microstructure, especially in normative aging. The results of our analysis, conducted on a large cohort of cognitively unimpaired adults, of the association between CBF and several MRI metrics of cerebral microstructural integrity, indicate that low CBF values correspond to low tissue integrity. These results provide further evidence of the intimate relationship between neurovascular physiology and brain integrity throughout normative aging.
|
|
| 14:54 | 0280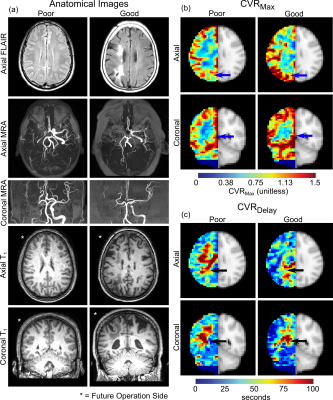 |
Time-delay processing of cerebrovascular reactivity reveals pre-surgical indicators of revascularization response in adults with moyamoya
Spencer L Waddle1, Maria E Garza1, Larry Taylor Davis2, Rohan Chitale2,3, Matthew Fusco2,3, Chelsea A Lee4, Niral J Patel4, Lori C Jordan1,2,4, and Manus J Donahue1,5
1Department of Neurology, Vanderbilt University Medical Center, Nashville, TN, United States, 2Department of Radiology and Radiological Sciences, Vanderbilt University Medical Center, Nashville, TN, United States, 3Department of Neurosurgery, Vanderbilt University Medical Center, Nashville, TN, United States, 4Department of Pediatrics, Division of Pediatric Neurology, Vanderbilt University Medical Center, Nashville, TN, United States, 5Department of Psychiatry and Behavioral Sciences, Vanderbilt University Medical Center, Nashville, TN, United States
The goal of this work is to apply time-regression analysis to hypercapnic reactivity data in an interventional trial to identify pre-surgical indicators of treatment response in moyamoya vasculopathy patients. We hypothesized that pre-surgical posterior flow-territory reactivity, including greater cerebrovascular reactivity and reduced vascular delay time, portend collateralization success. In 41 participants evaluated pre and 1-year post-operatively, pre-surgical posterior flow-territory maximum reactivity was higher (p=0.02) in patients with good vs. poor angiographic outcomes. This highlights that topographical features of preserved cerebral auto-regulation may contribute to neoangiogenic potential, and importantly, that reactivity mapping may provide a diagnostic tool for informing surgical candicacy.
|
|
| 15:06 | 0281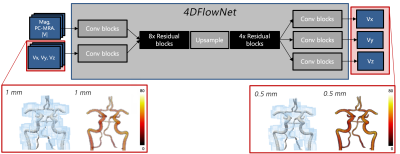 |
Intracranial super-resolution 4D Flow MRI – using deep-learning to map flow and relative pressure in the brain
David Marlevi1,2, Edward Ferdian3, Jonas Schollenberger4, Maria Aristova5, Brandon Hardy4, Elazer R Edelman1, Susanne Schnell5,6, C. Alberto Figueroa4, David A Nordsletten4,7, and Alistair A Young3,7
1Massachusetts Institute of Technology, Cambridge, MA, United States, 2Karolinska Institutet, Stockholm, Sweden, 3University of Auckland, Auckland, New Zealand, 4University of Michigan, Ann Arbor, MI, United States, 5Northwestern University, Chicago, IL, United States, 6University of Greifswald, Greifswald, Germany, 7King's College London, London, United Kingdom
Changes in regional hemodynamics are indicative of cerebrovascular disease. However, image-based monitoring is complicated by the unique flow and anatomies found in the brain, with accurate estimates requiring beyond state-of-the-art image resolutions. To address this, we combine a deep residual network, 4D Flow MRI, and physics-informed image processing to provide super-resolution flow images and coupled accurate quantification of intracranial relative pressure. The method is trained and validated on patient-specific in-silico data, highlighting how low resolution-biases are mitigated by super-resolution conversion. Data were also effectively generated at <0.5 mm in a representative in-vivo cohort, highlighting the potential of our presented approach.
|
|
| 15:18 | 0282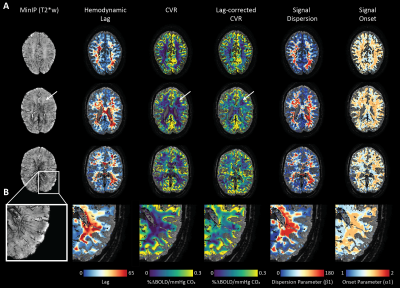 |
Medullary vein architecture modulates the white matter BOLD CVR response to CO2: observations from high-resolution T2* weighted imaging at 7T
Alex A Bhogal1
1UMC Utrecht, Utrecht, Netherlands
Brain stress testing using blood oxygenation level-dependent (BOLD) MRI to evaluate changes in cerebrovascular reactivity (CVR) is of growing interest for evaluating white matter integrity. However, even under healthy conditions, the white matter BOLD-CVR response differs notably from that observed in the gray matter. The confluence of arterial hemodynamics and BOLD signal characteristics weighted by venous architecture unrelated to smooth-muscle mediated dilation/contraction play a significant role in defining the WM BOLD-signal response to hypercapnia. This caveat should be taken into account when attributing disease mechanisms and/or progression to presumed impaired WM BOLD-CVR.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.