Weekend Course
Brain Tumors: From Molecules to MRI
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Current State of Brain Tumor Diagnosis | |||
| 13:00 | Genes & Molecules: Why Should We Care?
TBD
|
||
| 13:25 | Brain Tumors: A Tour of Current Clinical Practice
Mai-Lan Ho
This lecture will cover the imaging spectrum of adult and pediatric brain tumors with rich clinical case material, implementation of quantitative and advanced MRI techniques, and practical tips regarding diagnostic pearls and pitfalls. In addition, we will review key molecular pathways and genomic signatures relevant to patient diagnosis and management. Finally, we will introduce the concept of imaging genomics with examples of genotype-phenotype correlation, radiogenomics and deep learning, and emerging theranostic approaches.
|
||
| Moving Molecules: Perfusion & Diffusion | |||
| 13:50 | Perfusion MRI: How to Choose Between (& Within) Techniques
C. Chad Quarles
The overall purpose of this educational lecture is to discuss perfusion imaging options for brain tumor imaging. Topics will include protocol design informed by contrast mechanisms, sensitivity, and clinical utility. Emerging perfusion imaging techniques and their potential to aid in clinical decisions will also be discussed.
|
||
| 14:15 | Diffusion Within the Tumor Microenvironment
Markus Nilsson
This lecture will explain the link between tumor microstructure and the different parameters that we can observe with diffusion MRI.
|
||
| 14:40 | Break & Meet the Teachers |
||
| Static Molecules: CEST, MRS & X-Nuclei Imaging | |||
| 15:05 | 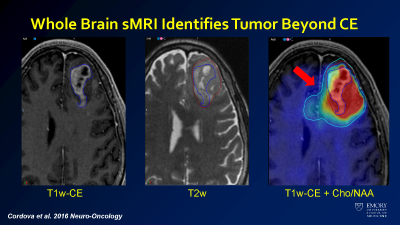 |
How to Measure Molecules in Brain Tumors & Why
Brent Weinberg, Hyunsuk Shim
Brain tumors are a challenging diagnosis that depend heavily on imaging, but routine MRI sequences including diffusion (DWI), FLAIR, and post-contrast T1 have their limitations. MRS has the capability to measure molecular concentrations non-invasively and without a contrast injection. Whole brain spectroscopic MRI (sMRI) has the potential to improve the clinical impact of MR spectroscopy on diagnosis and treatment of brain tumors by guiding surgical and radiation management in a way that can improve patient outcomes. Future developments may bring further applications of this technology beyond brain tumors and into other categories of disease.
|
|
| 15:30 | X-Nuclei Imaging in Brain Tumors
Tanja Platt
Physiologically relevant nuclei that enable MR applications ('X-nuclei') in tumor imaging in addition to hydrogen (1H) will be presented and the special MR characteristics of these nuclei will be explained. X-nuclei MR applications offer a wide variety of applications in science and translational research. Here, an overview of the physical MR properties of these nuclei and clinical research applications in brain tumor imaging will be given.
|
||
| Update on Treatment Options & How These Affect What We See on MRI | |||
| 15:55 | Treating Brain Tumors: What Can We Do (& Where Do We Still Fail)
Manabu Kinoshita
Surgical impact on overall survival for IDH-mutant tumors is much more significant than IDH-wildtype tumors. Thus, the role of neuroimaging is different between these two diseases. It is crucial to predict the presence or absence of IDH mutation, as it has a significant influence on the surgical strategies of the tumor. On the other hand, it is still difficult to fully visualize the full extension of the disease for IDH-wildtype tumors, which hinders planning the most efficient radiotherapy. The author would like to provide an overview of the current standard treatment strategies for gliomas, referring to the role of neuroimaging.
|
||
| 16:20 | Challenges in Imaging Treated Brain Tumors
Yae Won Park
The accurate assessment of glioma disease status is challenging due to the complex combination of therapies and treatment-related changes, along with the sometimes ambiguous and overlapping imaging findings. The history of response assessment in glioma – Macdonald, RANO, and mRANO – will be introduced and discussed. The posttreatment imaging findings, including pseudoprogression, radiation necrosis, pseudoresponse, and true progression, will be discussed. In short, this lecture will endeavor to aid the real-world imaging interpretation situation, where us radiologists must make our own decision on the posttreatment glioma MRI with the accessible information, and give the clinicians a satisfying answer. |
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.