Scientific Highlights of the ISMRM 27th Annual Meeting
Special Session: Scientific Highlights of the ISMRM 27th Annual Meeting
Plenary Session
Plenary Session
This session's recording is available to the public below.
Video begins with the YIA awards and the "Standardization in MRI: Why Is It So Challenging?" plenary session.
Thursday, 16 May 2019
| Plenary Hall - Room 517 | 11:45 - 12:15 | Moderators: Karla Miller, Scott Reeder |
| 11:45 |
1110.  |
First-in-human trial of Gd-based theranostic nanoparticles: MRI assessment of uptake and biodistribution in patients with multiple brain metastases
Sandrine Dufort, Camille Verry, Benjamin Lemasson, Sylvie Grand, Yannick Crémillieux, François Lux, Sébastien Mériaux, Benoit Larrat, Jacques Balosso, Géraldine Le Duc, Emmanuel Barbier, Olivier Tillement
We report here the main MRI findings of a dose escalation phase 1 clinical trial with intravenous administration of theranostic AGuIX nanoparticles, conducted in 15 patients with brain metastases with the objective of evaluating the efficacy of the nanoparticles as contrast agent and radiosensitizer for brain metastases. The nanoparticles were found to enhance four different histological types of brain metastases up to one week after nanoparticle administration. Quantitative measurements of nanoparticle concentration in all types of brain metastases were obtained two hours after administration to patient - and incidentally two hours before the first session of whole brain radiotherapy.
|
11:51 |
1111. 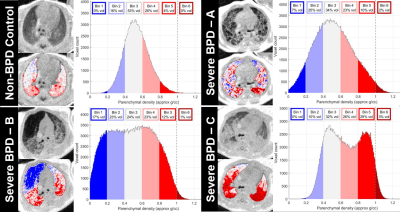 |
Objective lung-density quantification in neonatal bronchopulmonary dysplasia via ultrashort echo-time MRI, with comparison to clinical severity and reader scoring
Nara Higano, Robert Fleck, Andrew Schapiro, Andrew Hahn, Sean Fain, Melissa House, Paul Kingma, Jason Woods
Neonatal lung disease of prematurity (bronchopulmonary dysplasia, BPD) is a serious pulmonary condition. However, there is little understanding of the underlying structural pathologies or relationship to disease trajectories. Pulmonary MRI of neonatal BPD is an emerging research technique, with preliminary correlation to clinical outcomes, but assessment of parenchyma has been limited to manual radiological reads. We present quantitative lung-density measures in 55 patients from ultrashort echo-time (UTE) MRI, with strong correlation to clinical BPD severity and a current BPD reader scoring system. This technique distinguishes between patients with varying lung-density phenotypes, which in the future may help inform treatment strategies.
|
| 11:57 |
1112. 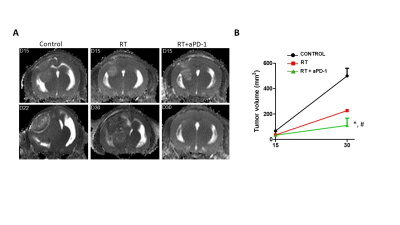 |
Longitudinal multimodal MRI monitoring of a novel combination therapy using radiosurgery and checkpoint inhibitor immunotherapy in glioblastoma multiforme
zhao jiang, Mariano Clausi, Alexander Stessin, Samuel Ryu, Timothy Duong
Multimodal MRI was used to longitudinally monitor the effects of a novel combination therapy of radiosurgery and programmed death-ligand 1 (PD-1) checkpoint inhibitor in a mouse model of GBM. We found that combination therapy of radiosurgery and immune checkpoint inhibition was more effective in reducing tumor volume and yielded better survival compared to non-treated, radiation-alone or immunotherapy-alone group. At 30-day post-treatment onset, tumor-ROI T2, apparent-diffusion coefficient, fractional anisotropy, and kurtosis of the combination treatment group were significantly different from those of the non-treated group (p<0.05). Immunohistochemical results further shed light on possible mechanisms of action.
|
12:03 |
1113. 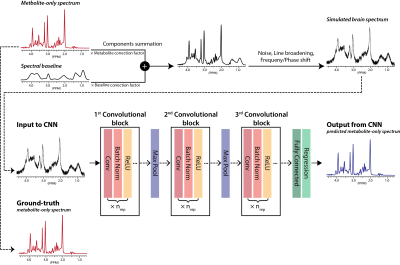 |
Intact Metabolite Spectrum Mining by Deep Learning in Proton Magnetic Resonance Spectroscopy of the Brain
HyeongHun Lee, Hyeonjin Kim
1H-MRS can quantify brain metabolites noninvasively. However, in a typical clinical setting, human brain spectra are indispensably degraded due to low SNR, line-broadening, and unknown spectral baseline, and consequently, quantification of brain metabolites is challenging even with the current state-of-the-art software. Given the recent accomplishment of deep-learning in a variety of different tasks, we developed a convolutional-neural-network (CNN) that maps the degraded brain spectra into noise-free, line-narrowed, baseline-removed, metabolite-only spectra. The robust performance of the proposed method as validated on both simulated and in vivo human brain spectra strongly supports the potential of deep learning in 1H-MRS of human brain.
|
12:09 |
1114. 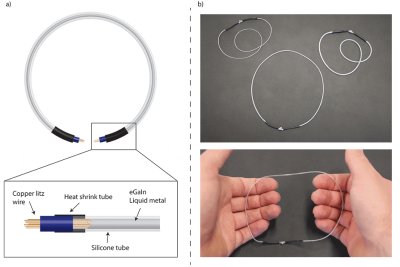 |
Liquid metal in stretchable tubes: A wearable 4-channel knee array
Andreas Port, Loris Albisetti, Matija Varga, Josip Marjanovic, Jonas Reber, David Brunner, Klaas Pruessmann
MR detectors that conform to individual patients and anatomy are a long-standing goal dating back to the 1980s. Rigid-adjustable and flexible coil designs have been proposed. The highest degree of wearability and adaptation is arguably achieved with stretchable coils. In this work, we present highly stretchable and lightweight receive coils realized by containing eutectic Gallium Indium liquid metal in silicone tubes. Particular emphasis is placed on assessing stretching behavior in terms of Q, SNR and integrity of liquid metal containment. Practical utility is explored with a 4-channel array implementation used to image flexion of the human knee at 3T.
|
Skip to 74:00 to view this session.
 Back to Program-at-a-Glance |
Back to Program-at-a-Glance |  Back to Top
Back to Top